Korean J Radiol.
2009 Aug;10(4):420-423. 10.3348/kjr.2009.10.4.420.
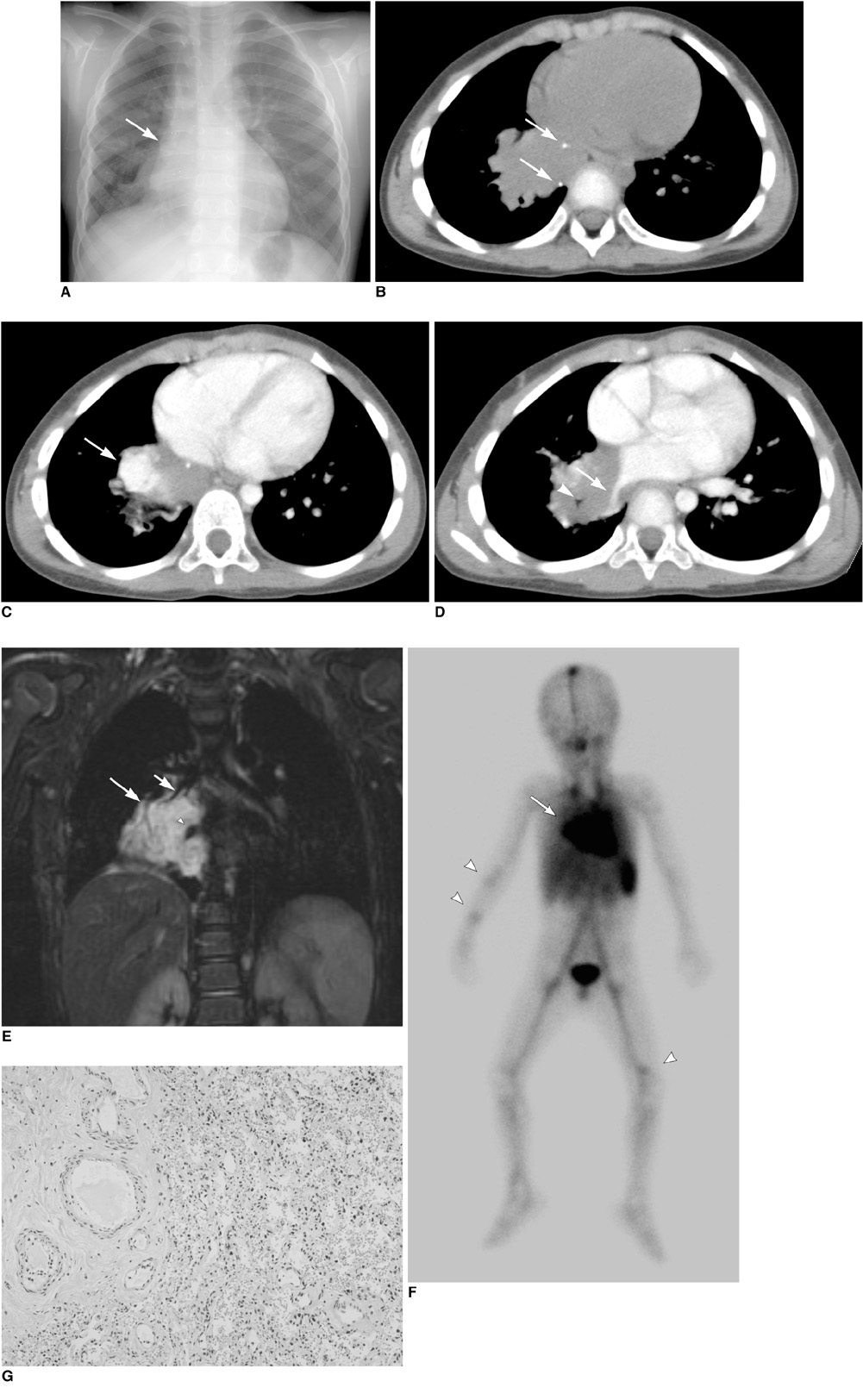
Pulmonary Venous Malformation in a 4-Year-Old Boy: a Case Report
- Affiliations
-
- 1Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul 110-746, Korea.
- 2Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea. jhrad@smc.samsung.co.kr
- 3Department of Pathology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea.
- 4Department of Thoracic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul 135-710, Korea.
- KMID: 1777274
- DOI: http://doi.org/10.3348/kjr.2009.10.4.420
Abstract
- We report a case of a pulmonary venous malformation in a 4-year-old boy who presented with recurrent pneumonia. A radiograph revealed a right infrahilar mass and a hyperlucent right lung. Computed tomography (CT) demonstrated a mass containing intensely enhancing areas and multiple phleboliths located in the right lower lobe and encasing the right bronchus and right inferior pulmonary vein. Magnetic resonance imaging (MRI) precisely revealed the mass demarcation. A right lower lobectomy was performed and a pathological examination confirmed the diagnosis of a venous malformation. To the best of our knowledge, a venous malformation in pulmonary tissue has not been reported in the English literature. Herein, we report a case of a pulmonary venous malformation, with the radiograph, CT, MRI, and blood pool scan findings, along with its pathologic correlation.
MeSH Terms
Figure
Reference
-
1. Legehn GM, Heran MK. Venous malformations: classification, development, diagnosis, and interventional radiologic management. Radiol Clin North Am. 2008. 46:545–597.2. Abernethy LJ. Classification and imaging of vascular malformations in children. Eur Radiol. 2003. 13:2483–2497.3. Panicek DM, Heitzman ER, Randall PA, Groskin SA, Chew FS, Lane EJ Jr, et al. The continuum of pulmonary developmental anomalies. Radiographics. 1987. 7:747–772.4. Puig S, Casati B, Staudenherz A, Paya K. Vascular low-flow malformations in children: current concepts for classification, diagnosis and therapy. Eur J Radiol. 2005. 53:35–45.5. Reid LM. Lung growth in health and disease. Br J Dis Chest. 1984. 78:113–134.6. Galliani CA, Beatty JF, Grosfeld JL. Cavernous hemangioma of the lung in an infant. Pediatr Pathol. 1992. 12:105–111.7. Wodenhouse GE. Hemangioma of the lung: a review of four cases, including two not previously reported, one of which was complicated by brain abscess due to H. influenzae. J Thorac Surg. 1948. 17:408–415.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Venous Malformation of the Pyriform Sinus Treated with Ethanol Sclerotherapy
- Levoatriocardinal Vein Combined with Pulmonary Venous Varix Mimicking Arteriovenous Malformations: A Case Report
- Congenital Cystic Adenomatoid Malformation Associated with Extralobar Pulmonary Sequestration: A case report
- A Case of Multiple Pulmonary Arteriovenous Malformation Treated with Coil Embolization
- Ruptured Cerebral Arteriovenous Malformation with Giant Venous Aneurysm: Case Report