Korean J Radiol.
2009 Aug;10(4):333-339. 10.3348/kjr.2009.10.4.333.
Detection of Residual Brain Arteriovenous Malformations after Radiosurgery: Diagnostic Accuracy of Contrast-Enhanced Three-Dimensional Time of Flight MR Angiography at 3.0 Tesla
- Affiliations
-
- 1Department of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea. cgchoi@amc.seoul.kr
- 2Department of Neurosurgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- KMID: 1777260
- DOI: http://doi.org/10.3348/kjr.2009.10.4.333
Abstract
OBJECTIVE
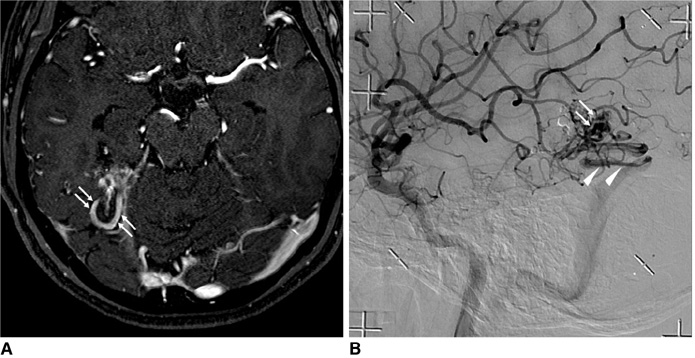
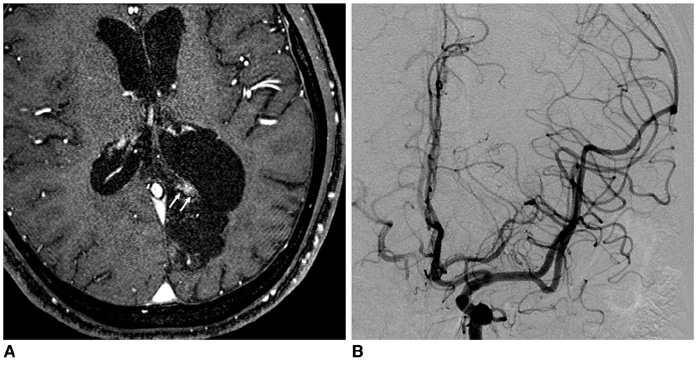
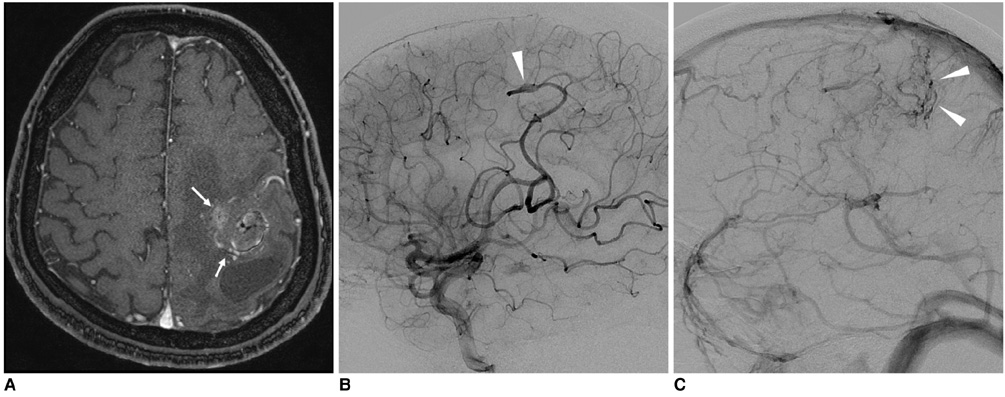
Although three-dimensional time-of-flight magnetic resonance angiography (3D TOF-MRA) is used frequently as a follow-up tool to assess the response of arteriovenous malformations (AVMs) after radiosurgery, the diagnostic accuracy of 3D TOF-MRA is not well known. We evaluated the diagnostic accuracy of contrast-enhanced 3D TOF-MRA at 3.0 Tesla for the detection of residual AVMs.
MATERIALS AND METHODS
This study included 32 AVMs from 32 patients who had been treated with radiosurgery (males/females: 21/11; average patient age, 33.1 years). The time interval between radiosurgery and MRA was an average of 35.3 months (range, 12-88 months). Three-dimensional TOF-MRA was obtained at a magnetic field strength of 3.0 Tesla after infusion of contrast media, with a measured voxel size of 0.40 x 0.80 x 1.4 (0.45) mm3 and a reconstructed voxel size of 0.27 x 0.27 x 0.70 (0.05) mm3 after zero-filling. X-ray angiography was performed as the reference of standard within six months after MRA (an average of two months). To determine the presence of a residual AVM, the source images of 3D TOF-MRA were independently reviewed, focusing on the presence of abnormally hyperintense fine tangled or tubular structures with continuity as seen on consecutive slices by two observers blinded to the X-ray angiography results.
RESULTS
A residual AVM was identified in 10 patients (10 of 32, 31%) on X-ray angiography. The inter-observer agreement for MRA was excellent (kappa= 0.813). For the detection of a residual AVM after radiosurgery as determined by observer 1 and observer 2, the source images of MRA had an overall sensitivity of 100%/90% (10 of 10, 9 of 10), specificity of 68%/68% (15 of 22, 15 of 22), positive predictive value of 59%/56% (10 of 17, 9 of 16), negative predictive value of 100%/94% (15 of 15, 15 of 16) and diagnostic accuracy of 78%/75% (25 of 32, 24 of 32), respectively.
CONCLUSION
The sensitivity of contrast-enhanced 3D TOF-MRA at 3.0 Tesla is high but the specificity is not sufficient for the detection of a residual AVM after radiosurgery.
MeSH Terms
Figure
Reference
-
1. Fleetwood IG, Steinberg GK. Arteriovenous malformations. Lancet. 2002. 359:863–873.2. Yamada S, Brauer FS, Colohan AR, Won DJ, Siddiqi J, Johnson WD, et al. Concept of arteriovenous malformation compartments and surgical management. Neurol Res. 2004. 26:288–300.3. Fournier D, TerBrugge KG, Willinsky R, Lasjaunias P, Montanera W. Endovascular treatment of intracerebral arteriovenous malformations: experience in 49 cases. J Neurosurg. 1991. 75:228–233.4. Lunsford LD, Kondziolka D, Flickinger JC, Bissonette DJ, Junqreis CA, Maitz AH, et al. Stereotactic radiosurgery for arteriovenous malformations of the brain. J Neurosurg. 1991. 75:512–524.5. Gobin YP, Laurent A, Merienne L, Schlienqer M, Aymard A, Houdart E, et al. Treatment of brain arteriovenous malformations by embolization and radiosurgery. J Neurosurg. 1996. 85:19–28.6. Schneider BF, Eberhard DA, Steiner LE. Histopathology of arteriovenous malformations after gamma knife radiosurgery. J Neurosurg. 1997. 87:352–357.7. Yamamoto M, Ide M, Jimbo M, Takakura K, Lindquist C, Steiner L. Neuroimaging studies of postobliteration nidus changes in cerebral arteriovenous malformations treated by gamma knife radiosurgery. Surg Neurol. 1996. 45:110–122.8. Yamamoto M, Jimbo M, Kobayashi M, Totoda C, Ide M, Tanaka N, et al. Long-term results of radiosurgery for arteriovenous malformation: neurodiagnostic imaging and histological studies of angiographically confirmed nidus obliteration. Surg Neurol. 1992. 37:219–230.9. Pollock BE, Lunsford LD, Kondziolka D, Maitz A, Flickinger JC. Patient outcomes after stereotactic radiosurgery for "operable" arteriovenous malformations. Neurosurgery. 1994. 35:1–7.10. Karlsson B, Lax I, Söderman M. Risk for hemorrhage during the 2-year latency period following gamma knife radiosurgery for arteriovenous malformations. Int J Radiat Oncol Biol Phys. 2001. 49:1045–1051.11. Maruyama K, Kawahara N, Shin M, Tago M, Kishimoto J, Kurita H, et al. The risk of hemorrhage after radiosurgery for cerebral arteriovenous malformations. N Engl J Med. 2005. 352:146–153.12. Kaufmann TJ, Huston J 3rd, Mandrekar JN, Schleck CD, Thielen KR, Kallmes DF. Complications of diagnostic cerebral angiography: evaluation of 19,826 consecutive patients. Radiology. 2007. 243:812–819.13. Heiserman JE, Dean BL, Hodak JA, Flom RA, Bird CR, Drayer BP, et al. Neurologic complications of cerebral angiography. AJNR Am J Neuroradiol. 1994. 15:1401–1407.14. Morikawa M, Numaguchi Y, Rigamonti D, Kuroiwa T, Rothman M, Zoarski G, et al. Radiosurgery for cerebral arteriovenous malformations: assessment of early phase magnetic resonance imaging and significance of gadolinium-DTPA enhancement. Int J Radiat Oncol Biol Phys. 1996. 34:663–675.15. Kauczor HU, Engenhart R, Layer G, Gamroth AH, Wowra B, Schad LR. 3D TOF MR angiography of cerebral arteriovenous malformations after radiosurgery. J Comput Assist Tomogr. 1993. 17:184–190.16. Mukherji SK, Quisling RG, Kubilis PS, Finn JP, Friedman WA. Intracranial arteriovenous malformations: quantitative analysis of magnitude contrast MR angiography versus gradient-echo MR imaging versus conventional angiography. Radiology. 1995. 196:187–193.17. Gauvrit JY, Oppenheim C, Nataf F, Naggara O, Trystram D, Munier T, et al. Three-dimensional dynamic magnetic resonance angiography for the evaluation of radiosurgically treated cerebral arteriovenous malformations. Eur Radiol. 2006. 16:583–591.18. Gaa J, Weidauer S, Requardt M, Kiefer B, Lanfermann H, Zanella FE. Comparison of intracranial 3D-TOF-MRA with and without parallel acquisition techniques at 1.5T and 3.0T: preliminary results. Acta Radiol. 2004. 45:327–332.19. Gibbs GF, Huston J 3rd, Bernstein MA, Riederer SJ, Brown RD Jr. Improved image quality of intracranial aneurysms: 3.0-T versus 1.5-T time-of-flight MR angiography. AJNR Am J Neuroradiol. 2004. 25:84–87.20. Hadizadeh DR, von Falkenhausen M, Gieseke J, Meyer B, Urbach H, Hoogeveen R, et al. Cerebral arteriovenous malformation: Spetzler-Martin classification at subsecond-temporalresolution four-dimensional MR angiography compared with that at DSA. Radiology. 2008. 246:205–213.21. Nagaraja S, Lee KJ, Coley SC, Capener D, Walton L, Kemeny AA, et al. Stereotactic radiosurgery for brain arteriovenous malformations: quantitative MR assessment of nidal response at 1 year and angiographic factors predicting early obliteration. Neuroradiology. 2006. 48:821–829.22. Pollock BE, Kondziolka D, Flickinger JC, Patel AK, Bissonette DJ, Lunsford LD. Magnetic resonance imaging: an accurate method to evaluate arteriovenous malformations after stereotactic radiosurgery. J Neurosurg. 1996. 85:1044–1049.23. Kihlström L, Guo WY, Karlsson B, Lindquist C, Lindqvist M. Magnetic resonance imaging of obliterated arteriovenous malformations up to 23 years after radiosurgery. J Neurosurg. 1997. 86:589–593.24. Guo WY, Lindquist C, Karlsson B, Kihlstrom L, Steiner L. Gamma knife surgery of cerebral arteriovenous malformations: serial MR imaging studies after radiosurgery. Int J Radiat Oncol Biol Phys. 1993. 25:315–323.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Role and Value of the MR Angiography of Vascular Lesion in the Brain : Comparative Analysis with Conventional Angiography
- Changes of MR Images in Arteriovenous Malformations of Brain after Gamma-knife Radiosurgery
- Artifacts in MR Angiography of the Intracranial Vessels Using the 3D TOF and 3D PC Techniques
- MR angiography of the renal arteries
- Radiosurgery for Intracranial Disorders