Yonsei Med J.
2011 May;52(3):539-542. 10.3349/ymj.2011.52.3.539.
The First Experience of Robot Assisted Spleen-Preserving Laparoscopic Distal Pancreatectomy in Korea
- Affiliations
-
- 1Division of Biliopancreas, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea. cmkang@yuhs.ac
- 2Pancreaticobiliary Cancer Clinic, Institute of Gastroenterology, Yonsei University Health System, Seoul, Korea.
- 3Department of Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 1777030
- DOI: http://doi.org/10.3349/ymj.2011.52.3.539
Abstract
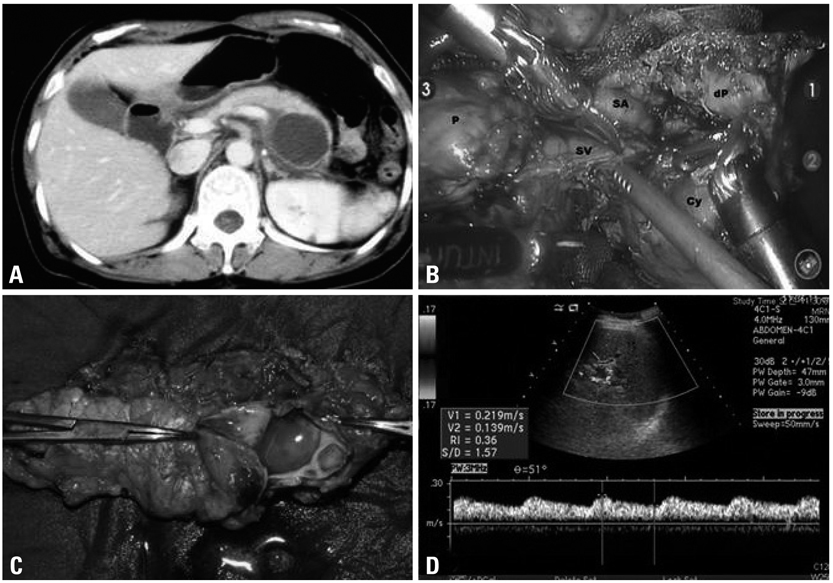
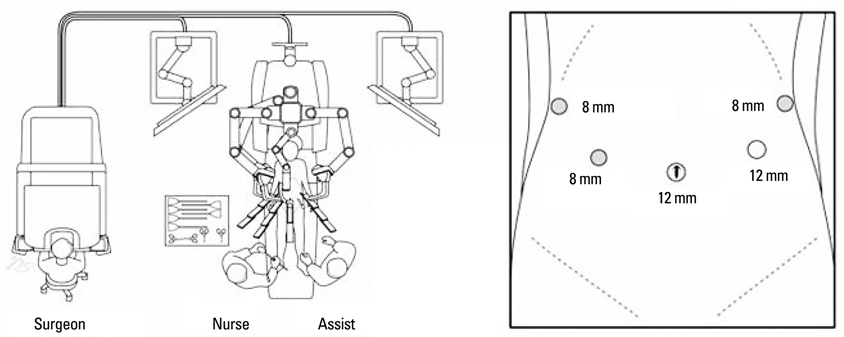
- Spleen-preservation has recently been emphasized in benign and borderline malignant pancreatic diseases requiring distal pancreatectomy. Reports to suggest that laparoscopic distal pancreatectomy is feasible and safe have been increasingly published. Robotic surgical system has been introduced and is expected to provide unique advantages in laparoscopic surgery. However, robot-assisted pancreatic surgery has not yet been performed by many surgeons. A 45-year-old female patient with abdominal discomfort was found to have pancreatic cyst in the body of the pancreas. Mucinous cystic tumor of the pancreas was the most favourable preoperative diagnosis. She underwent spleen-preserving laparoscopic distal pancreatectomy by using da Vinci surgical robot system. Splenic artery and vein were so tightly adherent to the pancreatic cyst that segmental resection of splenic vessels was required. Postoperative course was uneventful. She was able to come home in 5 days after surgery. Postoperative follow up color doppler ultrasound scan, taken on 2 weeks after surgery, showed minimal fluid collection around surgical field and no evidence of splenic infarction with good preservation of splenic perfusion. Robot-assisted spleen preserving distal pancreatectomy is thought to be feasible and safe. Several unique advantages of robotic system are expected to enhance safer and more precise surgical performance in near future. More experiences are mandatory to confirm real benefit of robot surgery in pancreatic disease.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Efficacy and Safety of Robotic Procedures Performed Using the da Vinci Robotic Surgical System at a Single Institute in Korea: Experience with 10000 Cases
Dong Hoon Koh, Won Sik Jang, Jae Won Park, Won Sik Ham, Woong Kyu Han, Koon Ho Rha, Young Deuk Choi
Yonsei Med J. 2018;59(8):975-981. doi: 10.3349/ymj.2018.59.8.975.
Reference
-
1. Sarr MG, Murr M, Smyrk TC, Yeo CJ, Fernandez-del-Castillo C, Hawes RH, et al. Primary cystic neoplasms of the pancreas. Neoplastic disorders of emerging importance-current state-of-the-art and unanswered questions. J Gastrointest Surg. 2003. 7:417–428.
Article2. Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC. The value of splenic preservation with distal pancreatectomy. Arch Surg. 2002. 137:164–168.
Article3. Sussman LA, Christie R, Whittle DE. Laparoscopic excision of distal pancreas including insulinoma. Aust N Z J Surg. 1996. 66:414–416.
Article4. Gagner M, Pomp A, Herrera MF. Early experience with laparoscopic resections of islet cell tumors. Surgery. 1996. 120:1051–1054.
Article5. Melvin WS, Needleman BJ, Krause KR, Ellison EC. Robotic resection of pancreatic neuroendocrine tumor. J Laparoendosc Adv Surg Tech A. 2003. 13:33–36.
Article6. Giulianotti PC, Coratti A, Angelini M, Sbrana F, Cecconi S, Balestracci T, et al. Robotics in general surgery: personal experience in a large community hospital. Arch Surg. 2003. 138:777–784.7. Takeuchi K, Tsuzuki Y, Ando T, Sekihara M, Hara T, Kori T, et al. Distal pancreatectomy: is staple closure beneficial? ANZ J Surg. 2003. 73:922–925.
Article8. Bilimoria MM, Cormier JN, Mun Y, Lee JE, Evans DB, Pisters PW. Pancreatic leak after left pancreatectomy is reduced following main pancreatic duct ligation. Br J Surg. 2003. 90:190–196.
Article9. Pannegeon V, Pessaux P, Sauvanet A, Vullierme MP, Kianmanesh R, Belghiti J. Pancreatic fistula after distal pancreatectomy: predictive risk factors and value of conservative treatment. Arch Surg. 2006. 141:1071–1076. discussion 6.10. Oláh A, Issekutz A, Belágyi T, Hajdú N, Romics L Jr. Randomized clinical trial of techniques for closure of the pancreatic remnant following distal pancreatectomy. Br J Surg. 2009. 96:602–607.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Dual-incision laparoscopic spleen-preserving distal pancreatectomy
- Laparoscopic Spleen Preserving Distal Pancreatectomy with the Conservation of the Splenic Artery and the Vein
- Splenic vessel patency: is it real menace to perform laparoscopic splenic vessel-preserving distal pancreatectomy
- Safety and Feasibility of Single Incision Laparoscopic Spleen Preserving Distal Pancreatectomy
- Initial Experiences using Robot-assisted Distal Pancreatectomy: A Single Institution Study of 28 Patients