Yonsei Med J.
2011 May;52(3):469-475. 10.3349/ymj.2011.52.3.469.
Clinical Observation Study of Massive Blood Transfusion in a Tertiary Care Hospital in Korea
- Affiliations
-
- 1Department of Laboratory Medicine, Chung Ang University College of Medicine, Seoul, Korea. ajcp@unitel.co.kr
- 2Department of Laboratory Medicine, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1777019
- DOI: http://doi.org/10.3349/ymj.2011.52.3.469
Abstract
- PURPOSE
Massive blood transfusios are uncommon. The goal of this study was to propose an ideal ratio for the blood component of massive hemorrhage treatment after review of five years of massive transfusion practice, in order to have the best possible clinical outcomes.
MATERIALS AND METHODS
We defined a 'massive transfusion' as receiving 10 or more units of red blood cells in one day. A list of patients receiving a massive transfusion from 2004 to 2008 was generated using the electronic medical records. For each case, we calculated the ratio of blood components and examined its relationship to their survival.
RESULTS
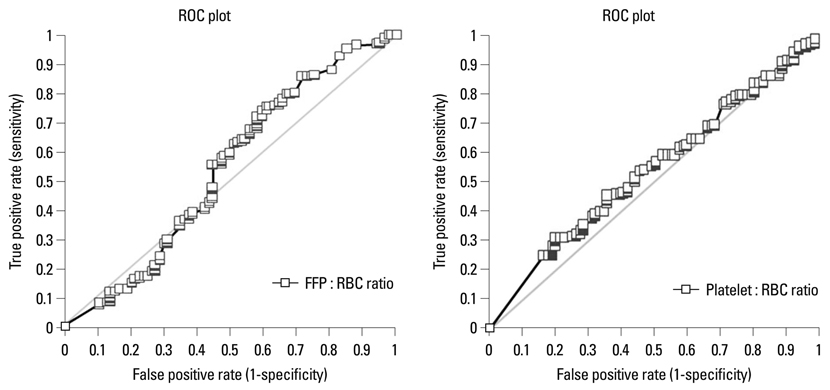
Three hundred thirty four patients underwent massive transfusion during the five years of the study. The overall seven-day hospital mortality for massive transfusion patients was 26.1%. Factors independently predictive of survival were a fresh-frozen plasma (FFP)/packed red blood cell (pRBC) ratio> or =1.1 with an odds ratio (OR) of 1.96 (1.03-3.70), and elective admission with an OR of 2.6 (1.52-4.40). The receiver operation characteristic (ROC) curve suggest that a 1 : 1 : 1 ratio of pRBCs to FFP to platelets is the best ratio for survival.
CONCLUSION
Fixing blood-component ratios during active hemorrhage shows improved outcomes. Thus, the hospital blood bank and physician hypothesized that a fixed blood component ratio would help to reduce mortality and decrease utilization of the overall blood component.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Massive Transfusion Protocols for Pediatric Patients
Hwan Tae Lee, Pil-Whan Park, Yiel-Hea Seo, Jeong-Yeal Ahn, Ja Young Seo, Ji-Hun Jeong, Moon Jin Kim, Jung Nam Lee, Gil Jae Lee, Kyung-Hee Kim
Lab Med Online. 2016;6(2):60-63. doi: 10.3343/lmo.2016.6.2.60.
Reference
-
1. John D. Roback, Brenda J. Grossman, Christopher D. Hillyer. Technical Manual. 2008. 16 ed. Maryland: America Association of Blood Banks.2. Malone DL, Hess JR, Fingerhut A. Massive transfusion practices around the globe and a suggestion for a common massive transfusion protocol. J Trauma. 2006. 60:S91–S96.
Article3. Rivers E, Nguyen B, Havstad S, Ressler J, Muzzin A, Knoblich B, et al. Early goal-directed therapy in the treatment of severe sepsis and septic shock. N Engl J Med. 2001. 345:1368–1377.
Article4. Riskin DJ, Tsai TC, Riskin L, Hernandez-Boussard T, Purtill M, Maggio PM, et al. Massive transfusion protocols: the role of aggressive resuscitation versus product ratio in mortality reduction. J Am Coll Surg. 2009. 209:198–205.
Article5. Borgman MA, Spinella PC, Perkins JG, Grathwohl KW, Repine T, Beekley AC, et al. The ratio of blood products transfused affects mortality in patients receiving massive transfusions at a combat support hospital. J Trauma. 2007. 63:805–813.
Article6. Bormanis J. Development of a massive transfusion protocol. Transfus Apher Sci. 2008. 38:57–63.
Article7. Johansson PI, Stensballe J. Effect of Haemostatic Control Resuscitation on mortality in massively bleeding patients: a before and after study. Vox Sang. 2009. 96:111–118.
Article8. Johansson PI, Bochsen L, Stensballe J, Secher NH. Transfusion packages for massively bleeding patients: the effect on clot formation and stability as evaluated by Thrombelastograph (TEG). Transfus Apher Sci. 2008. 39:3–8.
Article9. Johansson PI. The blood bank: from provider to partner in treatment of massively bleeding patients. Transfusion. 2007. 47:176S–181S.
Article10. Hardy JF, de Moerloose P, Samama CM. Massive transfusion and coagulopathy: pathophysiology and implications for clinical management. Can J Anaesth. 2006. 53:S40–S58.
Article11. Lee MK, Kim HO, Hong SG, Kwon OH, Kim JJ. Massive transfusion in Severance hospital. Korean J Blood Transfus. 1993. 4:23–28.12. Donaldson MD, Seaman MJ, Park GR. Massive blood transfusion. Br J Anaesth. 1992. 69:621–630.
Article13. Holcomb JB, Jenkins D, Rhee P, Johannigman J, Mahoney P, Mehta S, et al. Damage control resuscitation: directly addressing the early coagulopathy of trauma. J Trauma. 2007. 62:307–310.
Article14. Ketchum L, Hess JR, Hiippala S. Indications for early fresh frozen plasma, cryoprecipitate, and platelet transfusion in trauma. J Trauma. 2006. 60:S51–S58.
Article15. Kashuk JL, Moore EE, Johnson JL, Haenel J, Wilson M, Moore JB, et al. Postinjury life threatening coagulopathy: is 1:1 fresh frozen plasma:packed red blood cells the answer? J Trauma. 2008. 65:261–270.16. Scalea TM, Bochicchio KM, Lumpkins K, Hess JR, Dutton R, Pyle A, et al. Early aggressive use of fresh frozen plasma does not improve outcome in critically injured trauma patients. Ann Surg. 2008. 248:578–584.
Article17. Holcomb JB, Wade CE, Michalek JE, Chisholm GB, Zarzabal LA, Schreiber MA, et al. Increased plasma and platelet to red blood cell ratios improves outcome in 466 massively transfused civilian trauma patients. Ann Surg. 2008. 248:447–458.
Article18. Sperry JL, Ochoa JB, Gunn SR, Alarcon LH, Minei JP, Cuschieri J, et al. An FFP:PRBC transfusion ratio >/=1:1.5 is associated with a lower risk of mortality after massive transfusion. J Trauma. 2008. 65:986–993.
Article19. Hirshberg A, Dugas M, Banez EI, Scott BG, Wall MJ Jr, Mattox KL. Minimizing dilutional coagulopathy in exsanguinating hemorrhage: a computer simulation. J Trauma. 2003. 54:454–463.
Article20. Dunne JR, Riddle MS, Danko J, Hayden R, Petersen K. Blood transfusion is associated with infection and increased resource utilization in combat casualties. Am Surg. 2006. 72:619–625.
Article21. Sarani B, Dunkman WJ, Dean L, Sonnad S, Rohrbach JI, Gracias VH. Transfusion of fresh frozen plasma in critically ill surgical patients is associated with an increased risk of infection. Crit Care Med. 2008. 36:1114–1118.
Article22. Vamvakas EC. Platelet transfusion and postoperative infection in cardiac surgery. Transfusion. 2007. 47:352–354.
Article23. Gunter OL Jr, Au BK, Isbell JM, Mowery NT, Young PP, Cotton BA. Optimizing outcomes in damage control resuscitation: identifying blood product ratios associated with improved survival. J Trauma. 2008. 65:527–534.
Article24. Murphy GJ, Reeves BC, Rogers CA, Rizvi SI, Culliford L, Angelini GD. Increased mortality, postoperative morbidity, and cost after red blood cell transfusion in patients having cardiac surgery. Circulation. 2007. 116:2544–2552.
Article25. Khan H, Belsher J, Yilmaz M, Afessa B, Winters JL, Moore SB, et al. Fresh-frozen plasma and platelet transfusions are associated with development of acute lung injury in critically ill medical patients. Chest. 2007. 131:1308–1314.
Article26. Gonzalez EA, Moore FA, Holcomb JB, Miller CC, Kozar RA, Todd SR, et al. Fresh frozen plasma should be given earlier to patients requiring massive transfusion. J Trauma. 2007. 62:112–119.
Article27. Cotton BA, Au BK, Nunez TC, Gunter OL, Robertson AM, Young PP. Predefined massive transfusion protocols are associated with a reduction in organ failure and postinjury complications. J Trauma. 2009. 66:41–48.
Article28. O'Keeffe T, Refaai M, Tchorz K, Forestner JE, Sarode R. A massive transfusion protocol to decrease blood component use and costs. Arch Surg. 2008. 143:686–690.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative Analytical Study on Massive Transfusion between Traumatic Emergency and Existing Emergency Rooms for Traumatic Patients at a Tertiary Hospital
- A Simple Comment of Trauma-Induced Coagulopathy and Massive Transfusion
- Analysis of Massive Transfusion for Trauma Patients and Non-Trauma Patients in a Tertiary Hospital
- A Clinical Studies on Changes of Various Constitutions in the Blood after Massive Blood Transfusion
- Analysis of Application of Massive Transfusion Protocol for Trauma Patients at a Single Tertiary Referral Hospital