Korean J Gastroenterol.
2010 Dec;56(6):346-352. 10.4166/kjg.2010.56.6.346.
The Usefulness of Doppler Sonography in the Assessment of Disease Activity of Ulcerative Colitis
- Affiliations
-
- 1Department of Internal Medicine, The Catholic University College of Medicine, Seoul, Korea. jwchulkr@catholic.ac.kr
- 2Department of Radiology, The Catholic University College of Medicine, Seoul, Korea.
- KMID: 1775849
- DOI: http://doi.org/10.4166/kjg.2010.56.6.346
Abstract
- BACKGROUND/AIMS
Disease activity in ulcerative colitis (UC) is generally assessed using symptoms, laboratory data, endoscopic findings, and histology of the biopsy specimens. In this study, we compared disease activity of UC as determined by clinical features and endoscopic findings, and aimed to assess the clinical usefulness of Doppler sonography.
METHODS
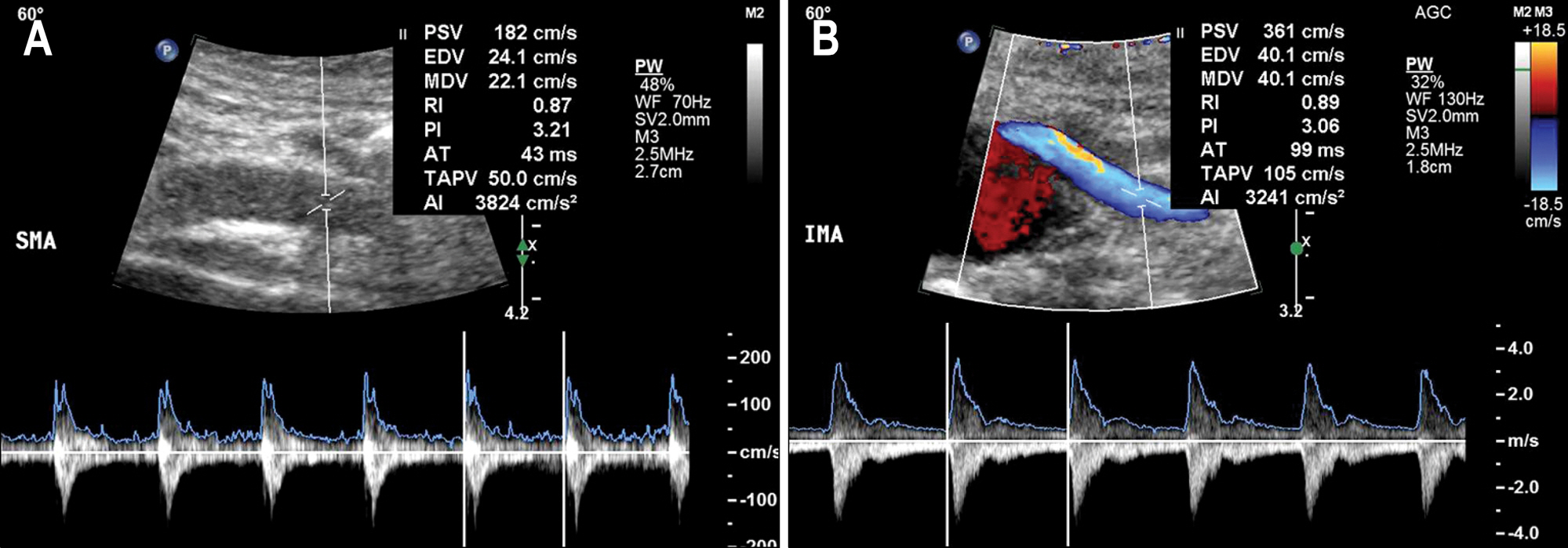
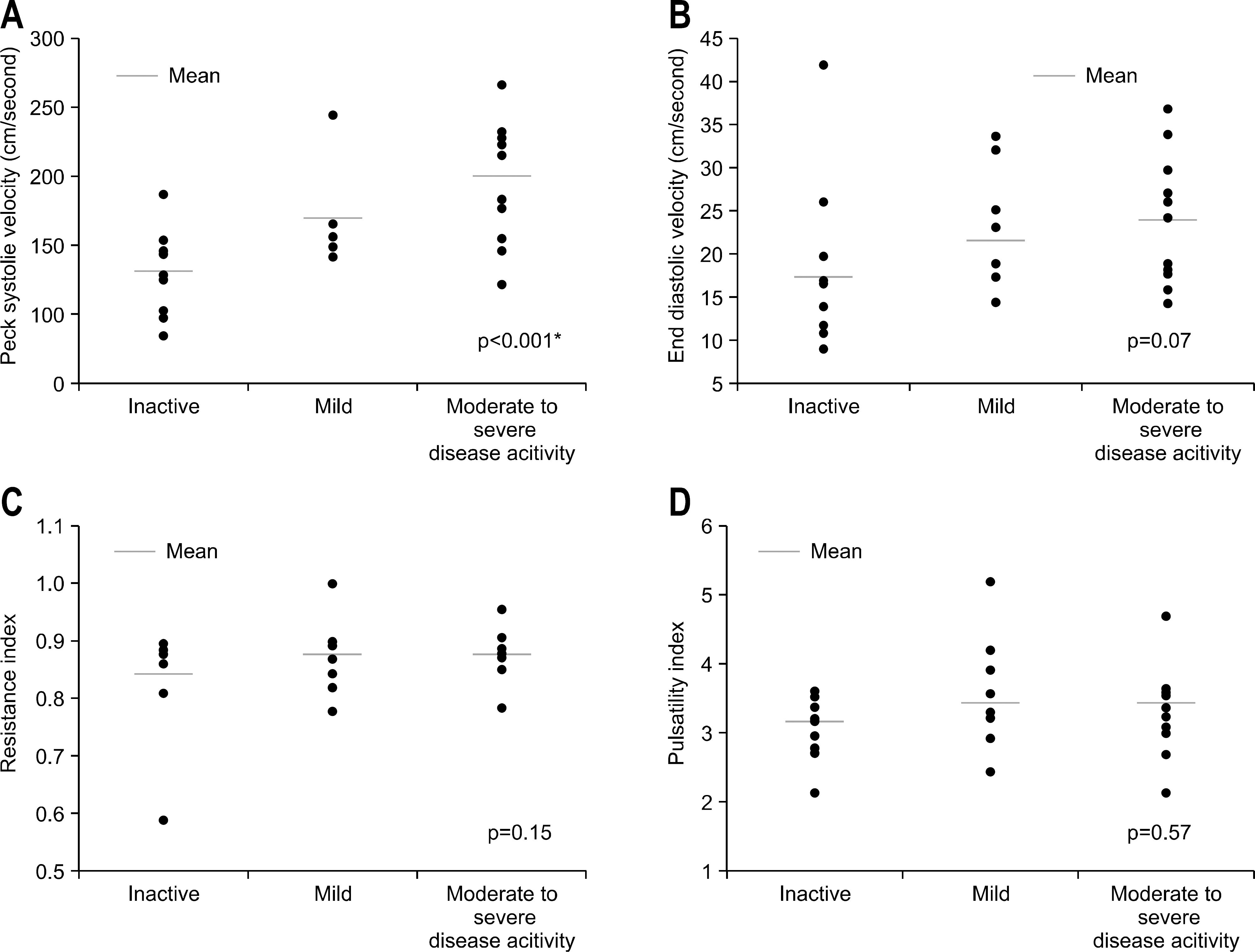
The duplex Doppler sonography of superior mesenteric artery (SMA) and inferior mesenteric artery (IMA) of 10 patients with clinically inactive UC and 20 patients with active UC were evaluated by one radiologist who was blinded to clinical information. Peak systolic velocity (PSV), end diastolic velocity (EDV), resistance index (RI), and pulsatility index (PI) of the SMA and IMA were evaluated. All patients underwent biochemical and endoscopic evaluations thereafter. Correlation between disease activity by the Truelove-Witts classification and the Mayo scoring system was measured, and we compared hemodynamic parameters between active and inactive UC.
RESULTS
Correlation rate of disease activity between these two scoring systems was 93.3%. Flow velocities (PSV, p<0.001 and EDV, p=0.03) and PI (p=0.03) were significantly higher in patients with active UC than inactive UC. PSVs of the SMA and IMA were also significantly correlated with disease severity. The active UC could be accurately diagnosed using Doppler sonography (AUC=0.83; 95% confidence interval 0.68-0.99).
CONCLUSIONS
In patients with UC, clinical stage was well matched with endoscopic disease activity. Doppler sonography was a readily available method, and PSV of SMA would be clinically useful in predicting of disease activity and severity.
Keyword
MeSH Terms
-
Adult
Aged
Area Under Curve
Blood Flow Velocity
Colitis, Ulcerative/pathology/*ultrasonography
Colonoscopy
Female
Humans
Male
Mesenteric Artery, Inferior/ultrasonography
Mesenteric Artery, Superior/ultrasonography
Middle Aged
ROC Curve
Sensitivity and Specificity
Severity of Illness Index
*Ultrasonography, Doppler, Duplex
Figure
Reference
-
1. Langholz E, Munkholm P, Davidsen M, Binder V. Course of ulcerative colitis: analysis of changes in disease activity over years. Gastroenterology. 1994; 107:3–11.
Article2. Ando T, Nishio Y, Watanabe O, et al. Value of colonoscopy for prediction of prognosis in patients with ulcerative colitis. World J Gastroenterol. 2008; 14:2133–2138.
Article3. Edwards FC, Truelove SC. The course and prognosis of ulcerative colitis. Gut. 1963; 4:299–315.4. Selby W. The natural history of ulcerative colitis. Baillieres Clin Gastroenterol. 1997; 11:53–64.5. Hiwatashi N, Yao T, Watanabe H, et al. Longterm follow-up study of ulcerative colitis in Japan. J Gastroenterol. 1995; 30(suppl 8):13–16.6. Truelove SC, Witts LJ. Cortisone in ulcerative colitis; final report on a therapeutic trial. Br Med J. 1955; 2:1041–1048.7. Naber AH, de Jong DJ. Assessment of disease activity in inflammatory bowel disease; relevance for clinical trials. Neth J Med. 2003; 61:105–110.8. Vermeire S, Van Assche G, Rutgeerts P. Laboratory markers in IBD: useful, magic, or unnecessary toys? Gut. 2006; 55:426–431.
Article9. Solem CA, Loftus EV Jr, Tremaine WJ, Harmsen WS, Zinsmeister AR, Sandborn WJ. Correlation of C-reactive protein with clinical, endoscopic, histologic, and radiographic activity in inflammatory bowel disease. Inflamm Bowel Dis. 2005; 11:707–712.
Article10. Hulté n L, Lindhagen J, Lundgren O, Fasth S, Ahré n C. Regional intestinal blood flow in ulcerative colitis and Crohn's disease. Gastroenterology. 1977; 72:388–396.
Article11. Ludwig D, Wiener S, Brü ning A, et al. Mesenteric blood flow is related to disease activity and risk of relapse in ulcerative colitis: a prospective follow up study. Gut. 1999; 45:546–552.
Article12. Di Sabatino A, Armellini E, Corazza GR. Doppler sonography in the diagnosis of inflammatory bowel disease. Dig Dis. 2004; 22:63–66.
Article13. Siğ irci A, Baysal T, Kutlu R, Aladağ M, Saraç K, Harput-luoğ lu H. Doppler sonography of the inferior and superior mesenteric arteries in ulcerative colitis. J Clin Ultrasound. 2001; 29:130–139.14. Fillinger MF, Schwartz RA. Volumetric blood flow measurement with color Doppler ultrasonography: the importance of visual clues. J Ultrasound Med. 1993; 12:123–130.
Article15. Schroeder KW, Tremaine WJ, Ilstrup DM. Coated oral 5-ami-nosalicylic acid therapy for mildly to moderately active ulcerative colitis. A randomized study. N Engl J Med. 1987; 317:1625–1629.16. Azzolini F, Pagnini C, Camellini L, et al. Proposal of a new clinical index predictive of endoscopic severity in ulcerative colitis. Dig Dis Sci. 2005; 50:246–251.
Article17. Rachmilewitz D. Coated mesalazine (5-aminosalicylic acid) versus sulphasalazine in the treatment of active ulcerative colitis: a randomised trial. BMJ. 1989; 298:82–86.
Article18. Baron JH, Conell AM, Lennard-Jones JE. Variation between observers in describing mucosal appearances in proctocolitis. Br Med J. 1964; 1:89–92.
Article19. Lee SD, Cohen RD. Endoscopy in inflammatory bowel disease. Gastroenterol Clin North Am. 2002; 31:119–132.
Article20. R⊘seth AG, Aadland E, Jahnsen J, Raknerud N. Assessment of disease activity in ulcerative colitis by faecal calprotectin, a novel granulocyte marker protein. Digestion. 1997; 58:176–180.
Article21. de Lange T, Larsen S, Aabakken L. Interobserver agreement in the assessment of endoscopic findings in ulcerative colitis. BMC Gastroenterol. 2004; 4:9.
Article22. Higgins PD, Schwartz M, Mapili J, Zimmermann EM. Is endoscopy necessary for the measurement of disease activity in ulcerative colitis? Am J Gastroenterol. 2005; 100:355–361.
Article23. Menees S, Higgins P, Korsnes S, Elta G. Does colonoscopy cause increased ulcerative colitis symptoms? Inflamm Bowel Dis. 2007; 13:12–18.
Article24. Gabay C, Kushner I. Acute-phase proteins and other systemic responses to inflammation. N Engl J Med. 1999; 340:448–454.
Article25. Zlonis M. The mystique of the erythrocyte sedimentation rate. A reappraisal of one of the oldest laboratory tests still in use. Clin Lab Med. 1993; 13:787–800.
Article26. Hilliard NJ, Waites KB. CME: C-reactive protein and ESR; What can one tell you that the other can't? Contemp Pediatr. 2002; 19:64–74.27. Ha JS, Lee JS, Kim HJ, et al. Comparative usefulness of erythrocyte sedimentation rate and C-reactive protein in assessing the severity of ulcerative colitis. Korean J Gastroenterol. 2006; 48:313–320.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Usefulness of Doppler Ultrasonography in Patients with Active Ulcerative Colitis
- Pathophysiology of ulcerative colitis - Relationship with genetics and immunity
- A Case of Hepatic Vein Thrombosis Associated with Ulcerative Colitis
- A Case of Cytomegalvirus Colitis Developed during the Treatment of Ulcerative Colitis
- A Case of Malignant Lymphoma in Patient with Ulcerative Colitis