Korean J Gastroenterol.
2013 Apr;61(4):203-208. 10.4166/kjg.2013.61.4.203.
Factors Associated with Vaccination among Inflammatory Bowel Disease Patients in Korea
- Affiliations
-
- 1Division of Gastroenterology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. younghokim@skku.edu
- KMID: 1775759
- DOI: http://doi.org/10.4166/kjg.2013.61.4.203
Abstract
- BACKGROUND/AIMS
Vaccinations are generally recommended in patients with inflammatory bowel disease (IBD). However, several studies showed low rates of vaccinations in IBD patients. Furthermore, vaccination rate among IBD patients in Korea has never been investigated. We investigated the vaccination rate among IBD patients in Korea and evaluated some factors that might affect the vaccination rate.
METHODS
From November 2011 to February 2012, a total of 192 patients with IBD who visited Samsung Medical Center (Seoul, Korea) answered the IRB-approved questionnaire. The questionnaire included their sex, age, residence, past medical history, type of IBD, duration of illness, medications, history of vaccination about measles-mumps-rubella (MMR), varicella, tetanus-diphtheria (Td), influenza, hepatitis A and B, pneumococcus and human papilloma virus (HPV).
RESULTS
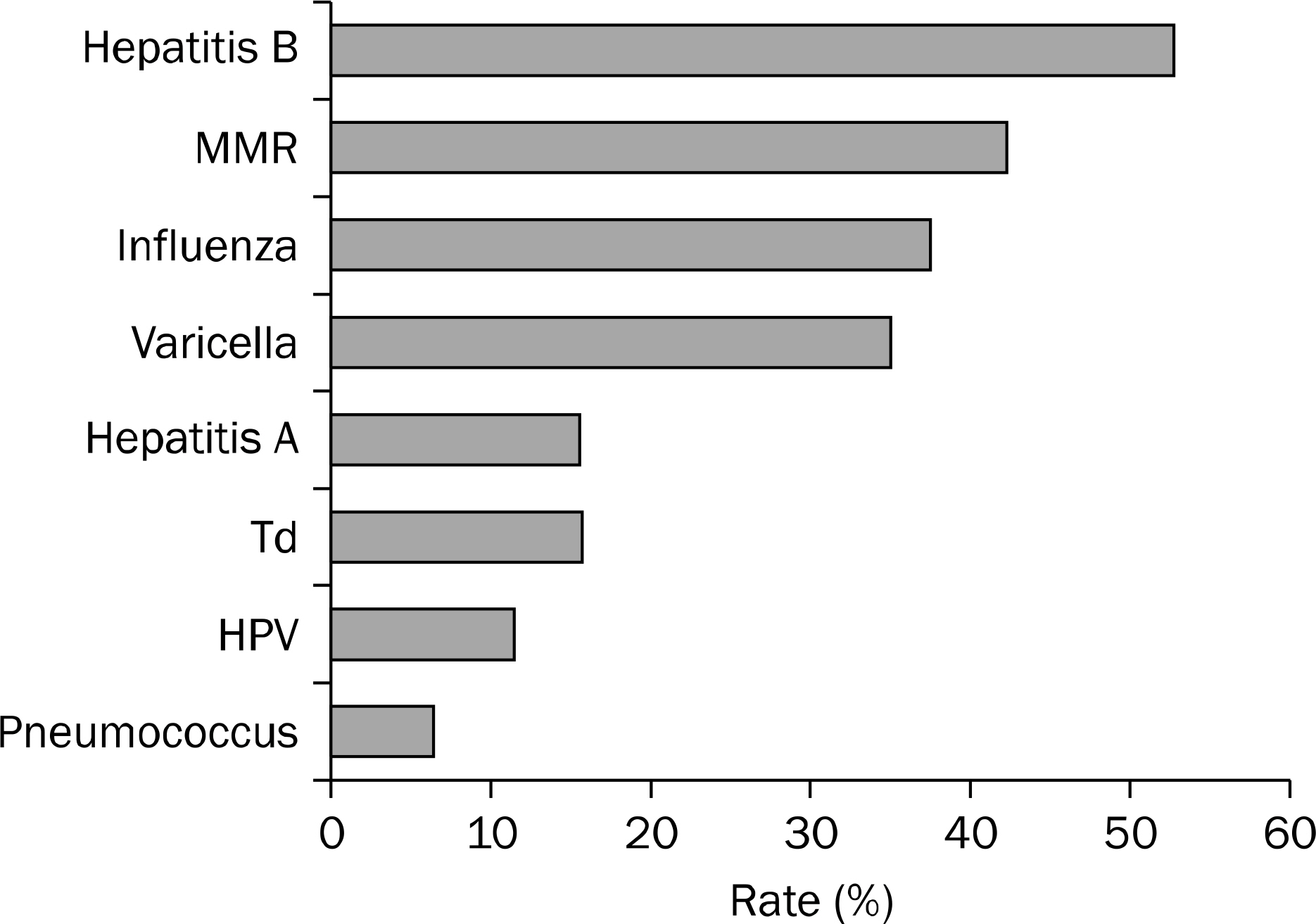
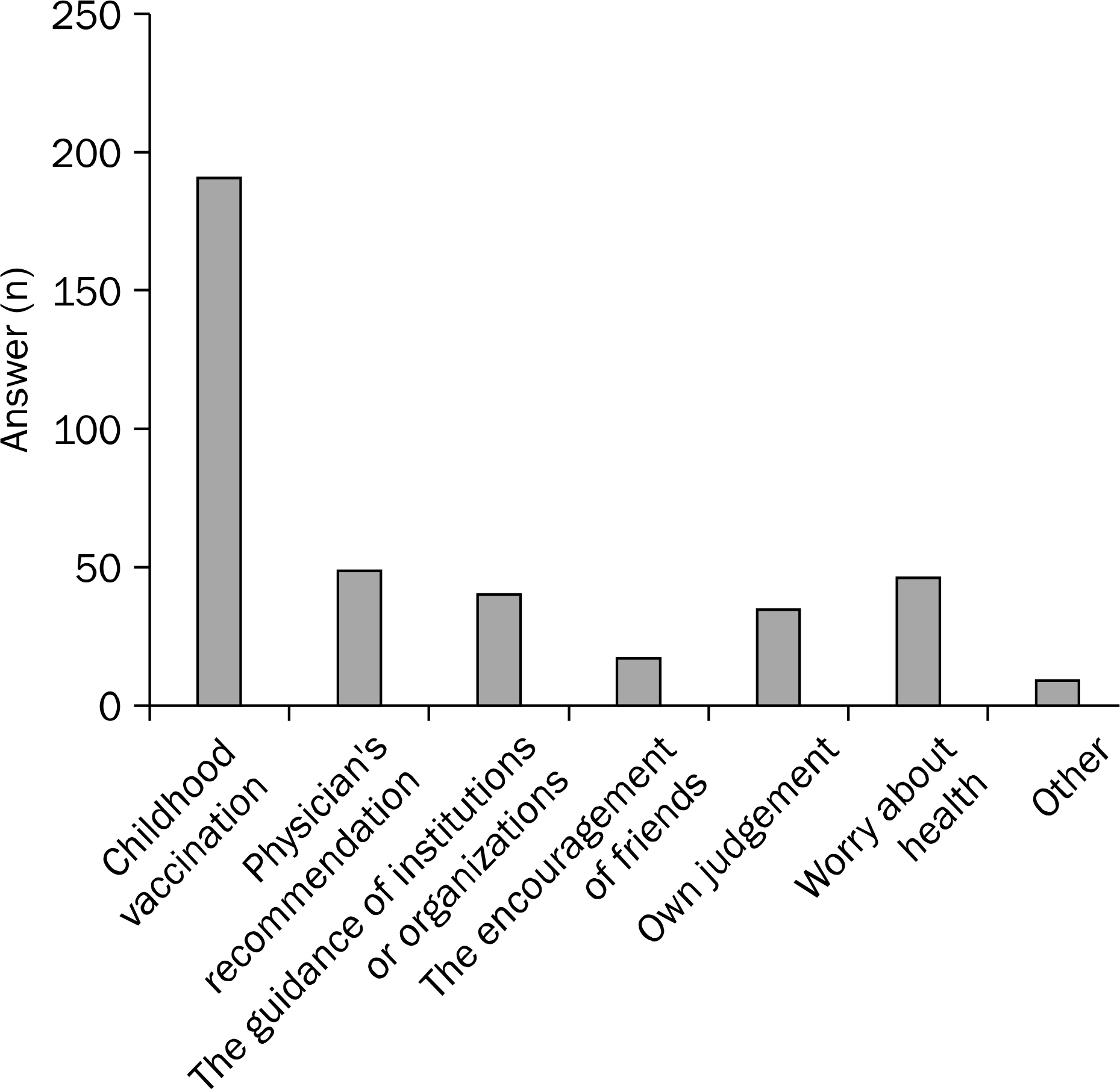
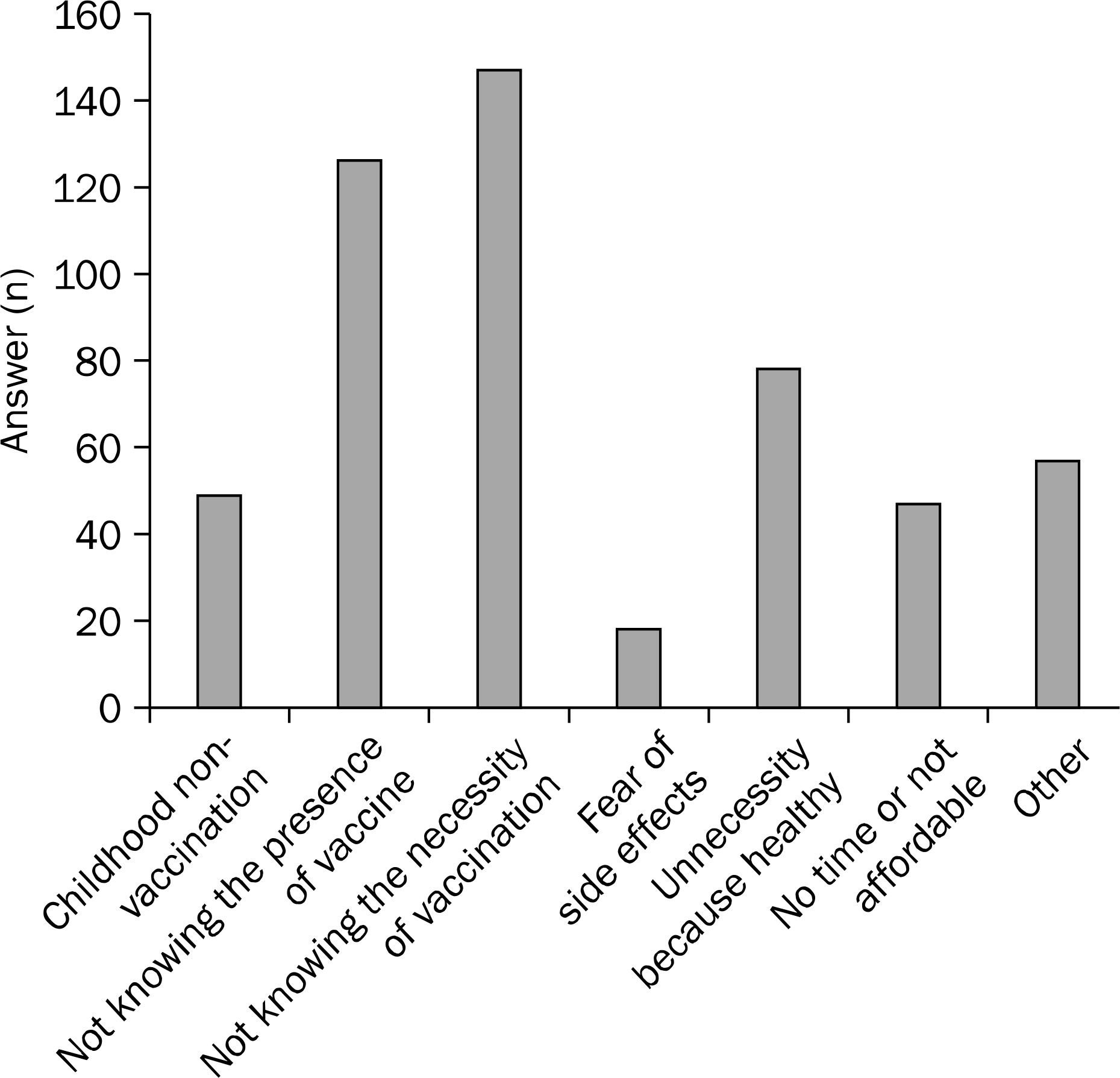
One hundred twenty one (63.0%) male and 71 (37.0%) female answered the questionnaire. The mean age of the enrolled patients was 39.7 (18-76) years. Eighty four patients (43.8%) had ulcerative colitis and 108 patients (56.3%) had Crohn's disease (CD). The percentage of the patients who had got vaccination was 42.2% for MMR, 34.9% for varicella, 15.6% for Td, 37.5% for influenza, 15.6% for hepatitis A, 52.6% for hepatitis B, 6.3% for pneumococcus and 11.3% for HPV respectively. Not knowing the necessity or the existence were the common reasons for non-vaccination. Age less than 40 years, CD patients and duration of illness less than 10 years were associated with a higher vaccination rate (p=0.002, 0.015 and 0.020, respectively).
CONCLUSIONS
Immunization rates for recommended vaccinations were very low in patients with IBD. Efforts to improve vaccination rate are needed.
MeSH Terms
-
Adolescent
Adult
Aged
Chickenpox/prevention & control
Colitis, Ulcerative/pathology
Crohn Disease/pathology
Diphtheria/prevention & control
Female
Hepatitis A/prevention & control
Hepatitis B/prevention & control
Humans
Inflammatory Bowel Diseases/*immunology/pathology
Male
Measles/prevention & control
Middle Aged
Mumps/prevention & control
Papillomavirus Infections/prevention & control
Pneumococcal Infections/prevention & control
Questionnaires
Republic of Korea
Rubella/prevention & control
Tetanus/prevention & control
*Vaccination
Young Adult
Figure
Cited by 3 articles
-
Ideal Vaccination Strategy in Inflammatory Bowel Disease
Chang Kyun Lee
Korean J Gastroenterol. 2015;65(3):159-164. doi: 10.4166/kjg.2015.65.3.159.Response to hepatitis B vaccination in patients with inflammatory bowel disease: a prospective observational study in Korea
Ji Young Chang, Sung-Ae Jung, Chang Mo Moon, Seong-Eun Kim, Hye-Kyung Jung, Ki-Nam Shim
Intest Res. 2018;16(4):599-608. doi: 10.5217/ir.2018.00012.Vaccination and Complementary and Alternative Medicine in Patients with Inflammatory Bowel Disease
Sung Bae Kim, Soo Jung Park, Sook Hee Chung, Kyu Yeon Hahn, Do Chang Moon, Sung Pil Hong, Jae Hee Cheon, Tae Il Kim, Won Ho Kim
Intest Res. 2014;12(2):124-130. doi: 10.5217/ir.2014.12.2.124.
Reference
-
References
1. Macdonald TT, Monteleone G. Immunity, inflammation, and allergy in the gut. Science. 2005; 307:1920–1925.
Article2. Keene JK, Lowe DK, Grosfeld JL, Fitzgerald JF, Gonzales-Crussi F. Disseminated varicella complicating ulcerative colitis. JAMA. 1978; 239:45–46.
Article3. Domm S, Cinatl J, Mrowietz U. The impact of treatment with tumour necrosis factoralpha antagonists on the course of chronic viral infections: a review of the literature. Br J Dermatol. 2008; 159:1217–1228.4. Bernal I, Domènech E, García-Planella E, Cabré E, Gassull MA. Opportunistic infections in patients with inflammatory bowel disease undergoing immunosuppressive therapy. Gastroenterol Hepatol. 2003; 26:19–22.5. Leung VS, Nguyen MT, Bush TM. Disseminated primary varicella after initiation of infliximab for Crohn's disease. Am J Gastroenterol. 2004; 99:2503–2504.
Article6. Mamula P, Markowitz JE, Piccoli DA, Klimov A, Cohen L, Baldassano RN. Immune response to influenza vaccine in pediatric patients with inflammatory bowel disease. Clin Gastroenterol Hepatol. 2007; 5:851–856.
Article7. Schattner A. Consequence or coincidence? The occurrence, pathogenesis and significance of autoimmune manifestations after viral vaccines. Vaccine. 2005; 23:3876–3886.8. Nielsen HJ, Mortensen T, Holten-Andersen M, Brünner N, Sørensen S, Rask-Madsen J. Increased levels of specific leuko- cyte- and platelet-derived substances during normal anti-teta-nus antibody synthesis in patients with inactive Crohn disease. Scand J Gastroenterol. 2001; 36:265–269.9. Sands BE, Cuffari C, Katz J, et al. Guidelines for immunizations in patients with inflammatory bowel disease. Inflamm Bowel Dis. 2004; 10:677–692.
Article10. Kotton CN. Vaccines and inflammatory bowel disease. Dig Dis. 2010; 28:525–535.
Article11. Melmed GY, Ippoliti AF, Papadakis KA, et al. Patients with inflammatory bowel disease are at risk for vaccine-preventable illnesses. Am J Gastroenterol. 2006; 101:1834–1840.
Article12. Loras C, Saro C, Gonzalez-Huix F, et al. Prevalence and factors related to hepatitis B and C in inflammatory bowel disease patients in Spain: a nationwide, multicenter study. Am J Gastroenterol. 2009; 104:57–63.13. Shim JJ, Chin SO, Lee CK, Jang JY, Kim BH. Epidemiological changes in hepatitis A in Korea: increasing age and its effect on clinical outcomes. Epidemiol Infect. 2012; 140:2182–2189.
Article14. Moleski SM, Choudhary C. Special considerations for women with IBD. Gastroenterol Clin North Am. 2011; 40:387–398.
Article15. Yang SK, Yun S, Kim JH, et al. Epidemiology of inflammatory bowel disease in the Songpa-Kangdong district, Seoul, Korea, 1986–2005: a KASID study. Inflamm Bowel Dis. 2008; 14:542–549.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vaccination strategies for Korean patients with inflammatory bowel disease
- Vaccination and Complementary and Alternative Medicine in Patients with Inflammatory Bowel Disease
- Response to hepatitis B vaccination in patients with inflammatory bowel disease: a prospective observational study in Korea
- Nutritional Support in Patients with Inflammatory Bowel Diseases
- The Pharmacotherapy of Inflammatory Bowel Disease in Child and Adolescence