Korean J Gastroenterol.
2013 Aug;62(2):135-139. 10.4166/kjg.2013.62.2.135.
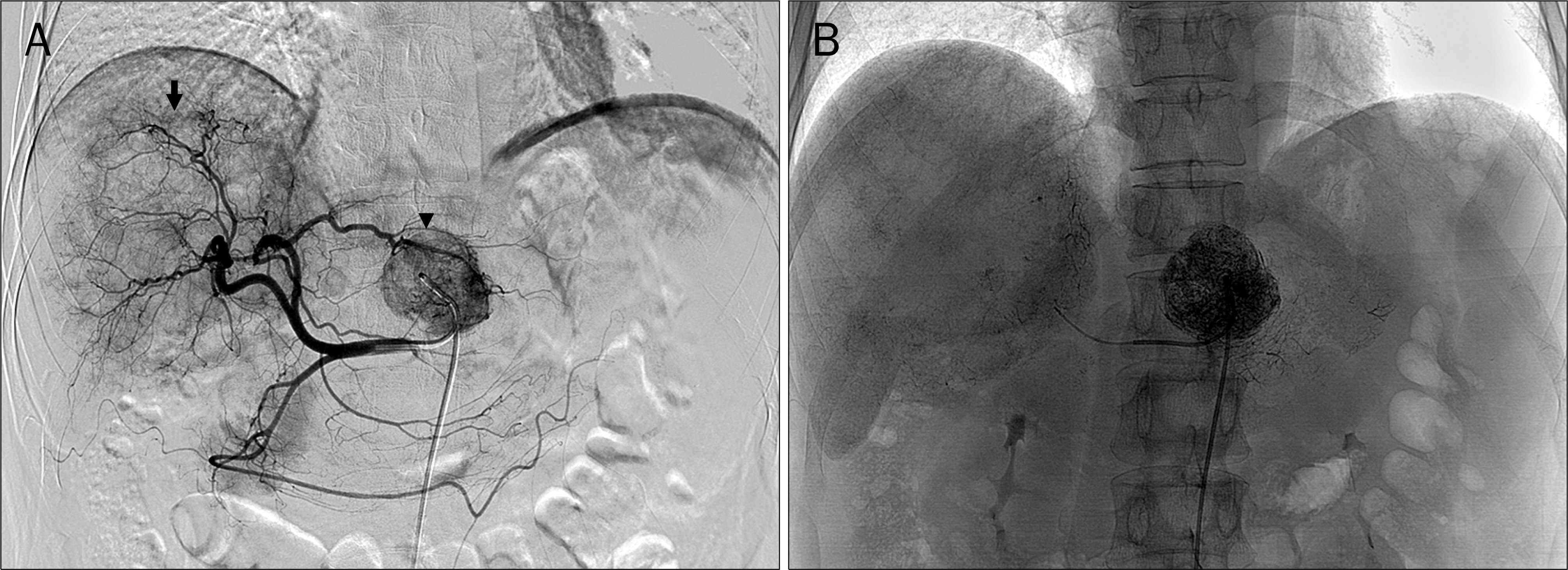
Synchronous Double Primary Hepatic Cancer: Hepatocellular Carcinoma and Intrahepatic Cholangiocarcinoma
- Affiliations
-
- 1Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea. noshin@hanyang.ac.kr
- 2Department of Pathology, Hanyang University College of Medicine, Seoul, Korea.
- KMID: 1775753
- DOI: http://doi.org/10.4166/kjg.2013.62.2.135
Abstract
- No abstract available.
MeSH Terms
-
Bile Duct Neoplasms/*diagnosis/pathology/radiography
Carcinoma, Hepatocellular/*diagnosis/radiography/therapy
Chemoembolization, Therapeutic
Cholangiocarcinoma/*diagnosis/pathology/radiography
Humans
Immunohistochemistry
Keratin-7/metabolism
Liver Neoplasms/*diagnosis/pathology/radiography/therapy
Male
Middle Aged
Neoplasms, Multiple Primary/*diagnosis/pathology/radiography
Positron-Emission Tomography
Tomography, X-Ray Computed
Keratin-7
Figure
Reference
-
References
1. Yano Y, Yamamoto J, Kosuge T, et al. Combined hepatocellular and cholangiocarcinoma: a clinicopathologic study of 26 resected cases. Jpn J Clin Oncol. 2003; 33:283–287.
Article2. Allen RA, Lisa JR. Combined liver cell and bile duct carcinoma. Am J Pathol. 1949; 25:647–655.3. Inaba K, Suzuki S, Sakaguchi T, et al. Double primary liver cancer (intrahepatic cholangiocarcinoma and hepatocellular carcinoma) in a patient with hepatitis C virus-related cirrhosis. J Hepatobiliary Pancreat Surg. 2007; 14:204–209.
Article4. Ohwada S, Yoshihiro O, Iwazaki S, et al. Double cancer in different hepatic lobes: hepatocellular and cholangiocellular carcinoma. Hepatogastroenterology. 1995; 42:411–414.5. Watanabe T, Sakata J, Ishikawa T, et al. Synchronous development of HCC and CCC in the same subsegment of the liver in a patient with type C liver cirrhosis. World J Hepatol. 2009; 1:103–109.
Article6. Fuji N, Taniguchi H, Amaike H, et al. Synchronously resected double primary hepatic cancer, hepatocellular carcinoma and cholangiocarcinoma. J Gastroenterol Hepatol. 2005; 20:967–969.
Article7. Matsuda M, Hara M, Suzuki T, Kono H, Fujii H. Synchronously resected double primary hepatic cancers – hepatocellular carcinoma and cholangiolocellular carcinoma. J Hepatobiliary Pancreat Surg. 2006; 13:571–576.
Article8. Sanada Y, Shiozaki S, Aoki H, Takakura N, Yoshida K, Yamaguchi Y. A clinical study of 11 cases of combined hepatocellular-cholangiocarcinoma Assessment of enhancement patterns on dynamics computed tomography before resection. Hepatol Res. 2005; 32:185–195.9. Park SY, Kim HS, Hong EK, Kim WH. Expression of cytokeratins 7 and 20 in primary carcinomas of the stomach and colorectum and their value in the differential diagnosis of metastatic carcinomas to the ovary. Hum Pathol. 2002; 33:1078–1085.
Article10. Kang DB, Kim SH, Byun SJ, et al. Metastatic small bowel perforation caused by intrahepatic cholangiocarcinoma in a patient with combined hepatocellular-cholangiocarcinoma. J Korean Surg Soc. 2009; 77:138–142.
Article11. Choi JH. Combined hepatocellular-cholangiocarcinoma: recent progress in pathology and classification. Yeungnam Univ J Med. 2011; 28:1–12.
Article12. Yin X, Zhang BH, Qiu SJ, et al. Combined hepatocellular carcinoma and cholangiocarcinoma: clinical features, treatment modalities, and prognosis. Ann Surg Oncol. 2012; 19:2869–2876.
Article13. Jarnagin WR, Weber S, Tickoo SK, et al. Combined hepatocellular and cholangiocarcinoma: demographic, clinical, and prognostic factors. Cancer. 2002; 94:2040–2046.14. Koh KC, Lee H, Choi MS, et al. Clinicopathologic features and prognosis of combined hepatocellular cholangiocarcinoma. Am J Surg. 2005; 189:120–125.
Article15. Lee CH, Hsieh SY, Chang CJ, Lin YJ. Comparison of clinical characteristics of combined hepatocellular-cholangiocarcinoma and other primary liver cancers. J Gastroenterol Hepatol. 2013; 28:122–127.
Article16. Singh S, Chakraborty S, Bonthu N, Radio S, Hussain SM, Sasson A. Combined hepatocellular cholangiocarcinoma: a case report and review of literature. Dig Dis Sci. 2013; 58:2114–2123.
Article17. Chi M, Mikhitarian K, Shi C, Goff LW. Management of combined hepatocellular-cholangiocarcinoma: a case report and literature review. Gastrointest Cancer Res. 2012; 5:199–202.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case Report of Synchronous Double Primary Liver Cancers Combined with Early Gastric Cancer
- A case with intrahepatic double cancer: hepatocellular carcinoma and cholangiocarcinoma associated with multiple von Meyenburg complexes
- Intermediate hepatic carcinoma mimicking intrahepatic cholangiocarcinoma: A case report
- Cancer Stem Cells in Primary Liver Cancers: Pathological Concepts and Imaging Findings
- Combined Hepatocellular-cholangiocarcinoma