Korean Circ J.
2009 Jan;39(1):32-36. 10.4070/kcj.2009.39.1.32.
Spontaneous Retroperitoneal Hemorrhage and Hemothorax After Intravenous Heparin Treatment
- Affiliations
-
- 1Division of Cardiology, Department of Internal Medicine, Cheongju St. Mary's Hospital, Cheongju, Korea.
- 2Division of Cardiology, Department of Internal Medicine, Soonchunhyang University Cheonan Hospital, Cheonan, Korea. drlsj@paran.com
- KMID: 1769511
- DOI: http://doi.org/10.4070/kcj.2009.39.1.32
Abstract
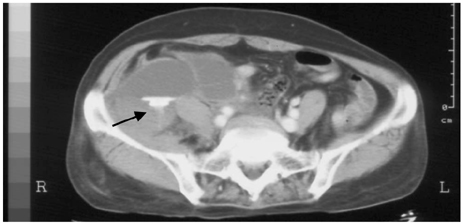
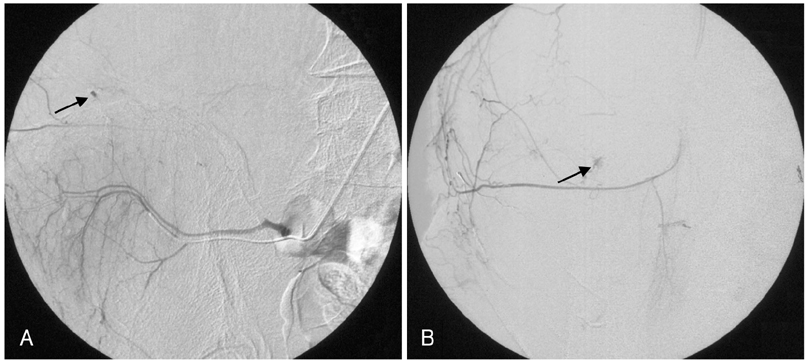
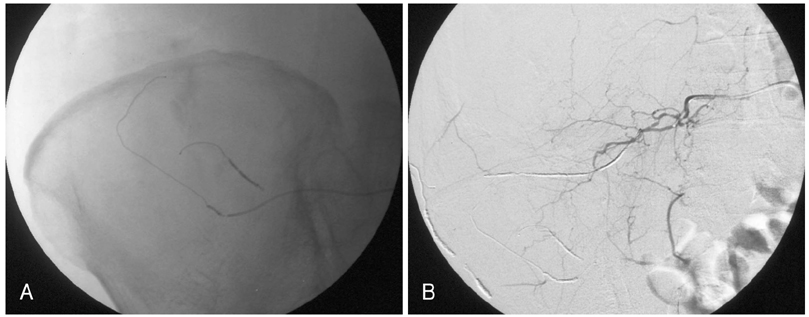
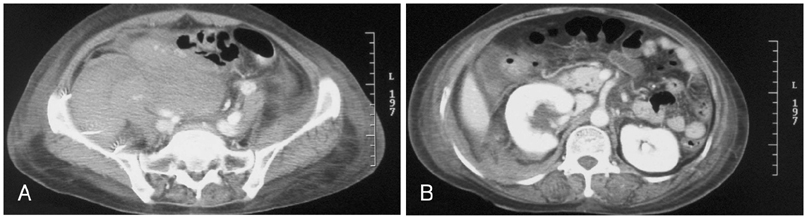
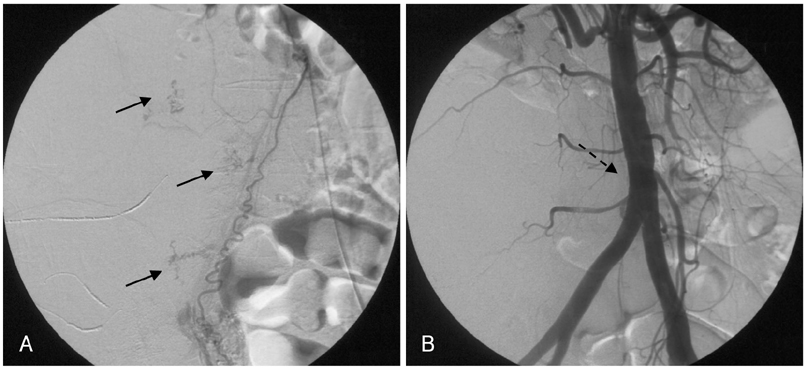
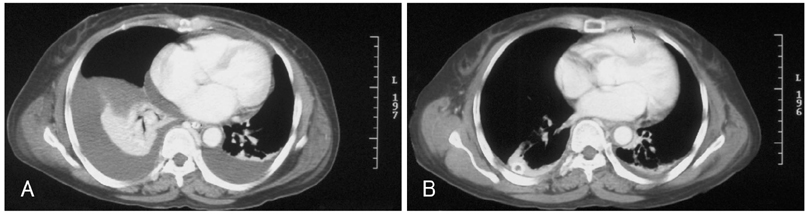
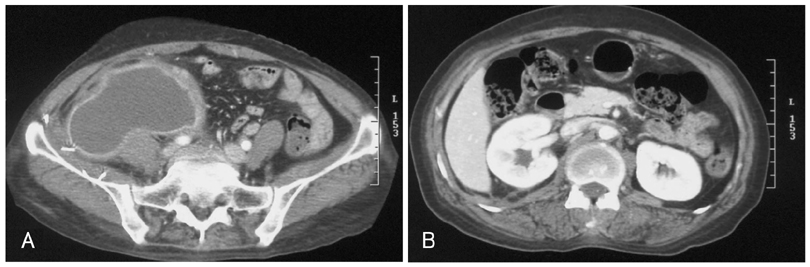
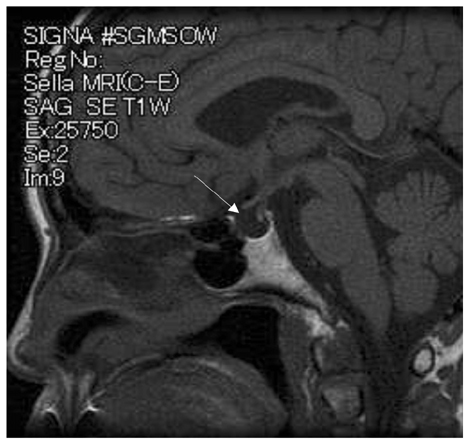
- Spontaneous retroperitoneal hemorrhage is a rare complication after percutaneous coronary intervention (PCI). The patient can be in danger if bleeding is not stopped immediately. However, it is not easy to control the bleeding completely because the bleeding foci can be multiple and there is a rich network of collateral circulation. We report a case of spontaneous retroperitoneal hemorrhage successfully treated using multiple microcoils. One year later, panhypopituitarism occurred as a likely consequence of the accompanying hypovolemic shock.
Keyword
MeSH Terms
Figure
Reference
-
1. Tappe U, Kristen F, Löffler A, Keller HW. Spontaneous retroperitoneal hematoma in adrenal metastasis. Dtsch Med Wochenschr. 1997. 122:471–474.2. Malik A, Capling R, Bastani B. Enoxaparin-associated retroperitoneal bleeding in two patients with renal insufficiency. Pharmacotherapy. 2005. 25:769–772.3. Ishihara S, Yasuhara H, Ogawa S, Muto T. Successful surgical treatment for spontaneous retroperitoneal hematoma in polycythemia vera: report of a case. Surg Today. 2000. 30:199–201.4. Jeong TK, Jeong GH, Park BS, et al. Dalteparin sodium-associated retroperitoneal hematoma in a patient with diabetic nephropathy. Korean J Med. 2003. 64:322–327.5. Kim HJ, Kim DY, Whang MG, Jo HK. A case of spontaneous retroperitoneal hemorrhage due to iliopsoas muscle hematoma in patient with myocardial infarction receiving intravenous heparin. Korean Circ J. 1998. 28:1798–1801.6. Sreeram S, Lumsden AB, Miller JS, Salam AA, Dodson TF, Smith RB. Retroperitoneal hematoma following femoral arterial catheterization: a serious and often fatal complication. Am Surg. 1993. 59:94–98.7. Chan YC, Morales JP, Reidy JF, Taylor PR. Management of spontaneous and iatrogenic retroperitoneal hemorrhage: conservative management, endovascular intervention or open surgery? Int J Clin Pract. 2007. [Epub ahead of print].8. Baker BH, Baker MS. Indications for exporing the retroperitoneal space. South Med J. 1980. 73:969–970.9. Grimm MR, Vrahas MS, Thromas KA. Pressure-volume characteristics of the intact and disrupted pelvic retroperitoneum. J Trauma. 1998. 44:454–459.10. Kauppila LI. Blood supply of the lower thoracic and lumbosacral regions: postmorterm aortography in 38 young adults. Acta Radiol. 1994. 35:541–544.11. Torres GM, Cernigliaro JG, Abbitt PL, et al. Iliopsoas compartment: normal anatomy and pathologic processes. Radiographics. 1995. 15:1285–1297.12. McCort JJ. Intraperitoneal and retroperitoneal hemorrhage. Radiol Clin North Am. 1976. 14:391–405.13. Berna JD, Zuazu I, Madrigal M, et al. Conservative treatment of large rectus sheath hematoma in patients undergoing anticoagulant therapy. Abdom Imaging. 2000. 25:230–234.14. Dabney A, Bastani B. Enoxaparin-associated severe retroperitoneal bleeding and abdominal compartment syndrome: a report of two cases. Intensive Care Med. 2001. 27:1954–1957.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Spontaneous Retroperitoneal Hemorrhage due to Iliopsoas Muscle Hematoma in Patient with Myocardial Infarction Receiving Intravenous Heparin
- Transcatheter Arterial Embolization as Treatment for a Life-Threatening Retroperitoneal Hemorrhage Complicating Heparin Therapy
- Spontaneous Retroperitoneal Hemorrhage from Ruptured Suprarenal Artery Aneurysm
- A Case of Spontaneous Hemo-pneumothorax
- A Case of Hemorrhagic Fever with Renal Syndrome Complicated by Retroperitoneal Hematoma and Hemothorax