Korean J Radiol.
2002 Mar;3(1):64-73. 10.3348/kjr.2002.3.1.64.
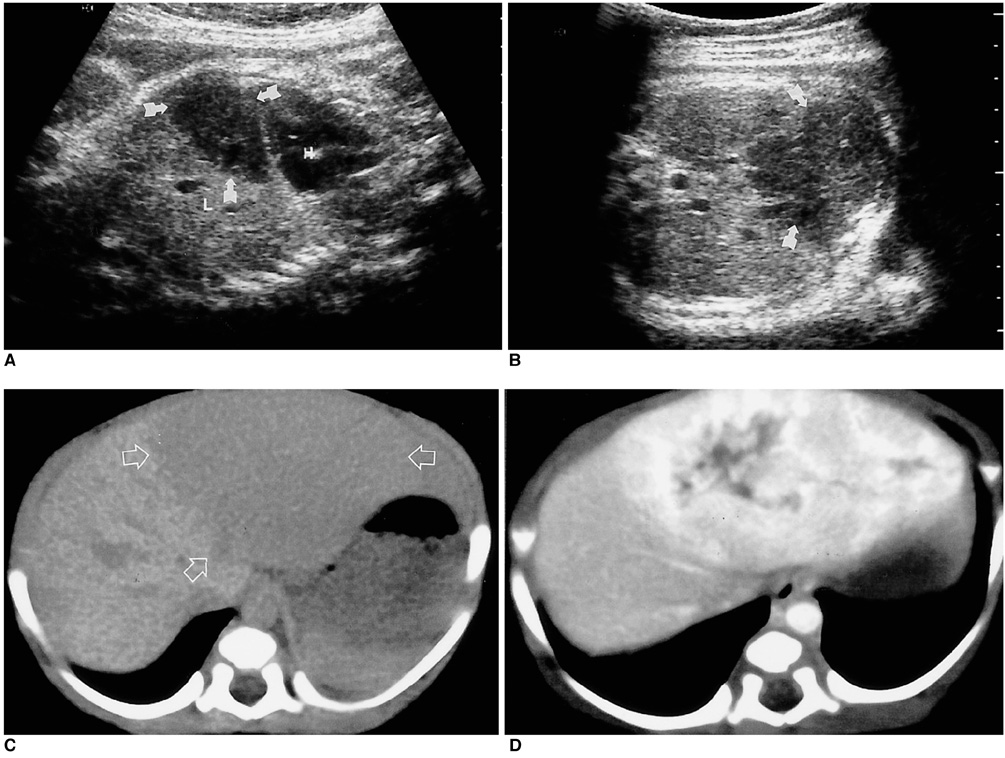
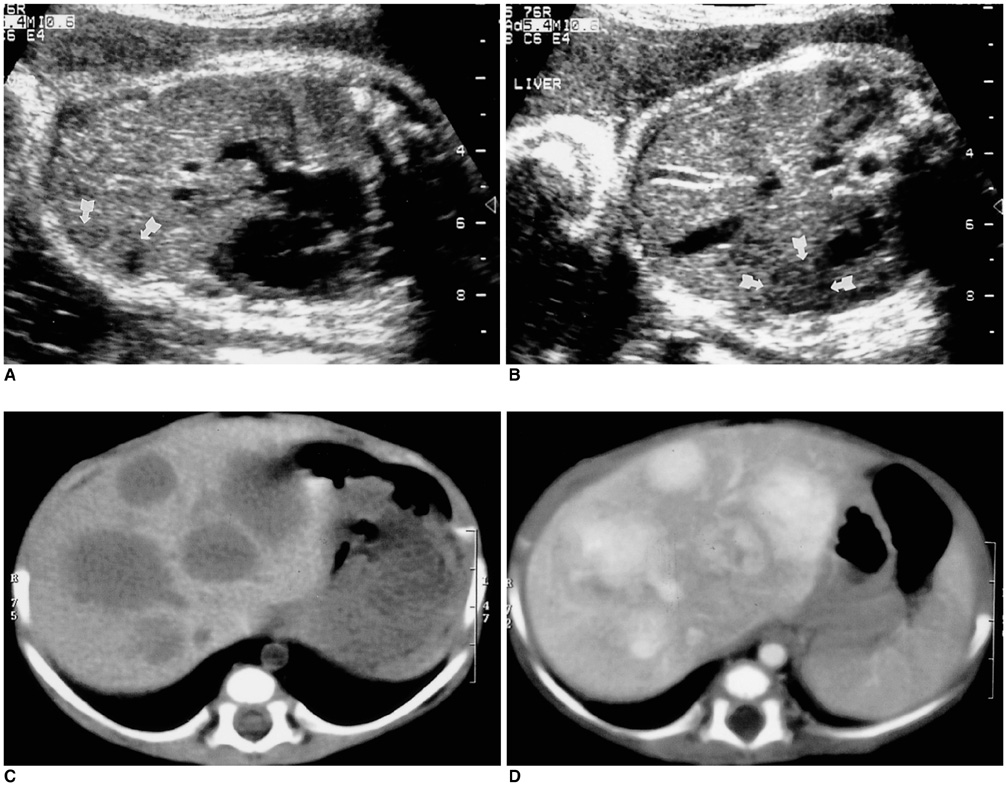
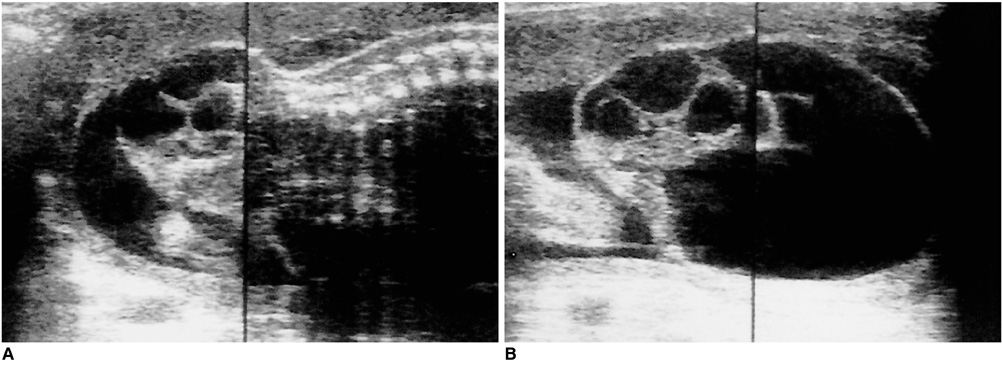
Prenatal Ultrasound Findings of Fetal Neoplasms
- Affiliations
-
- 1Department of Radiology, Samsung Cheil Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. radjycho@samsung.co.kr
- 2Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1758449
- DOI: http://doi.org/10.3348/kjr.2002.3.1.64
Abstract
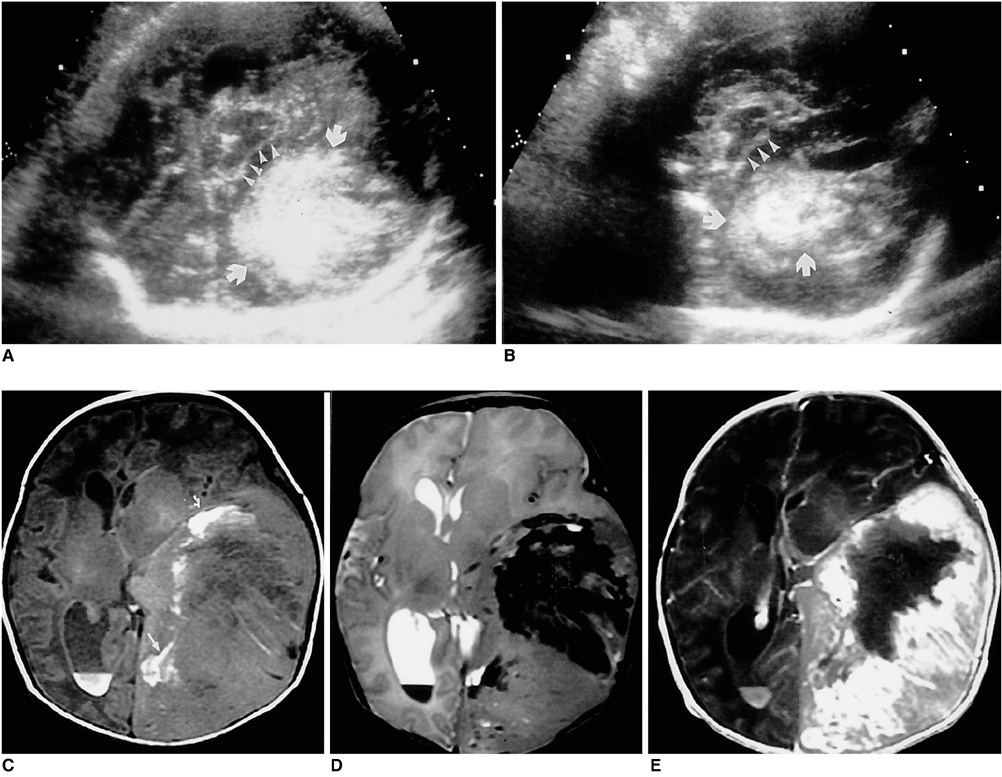
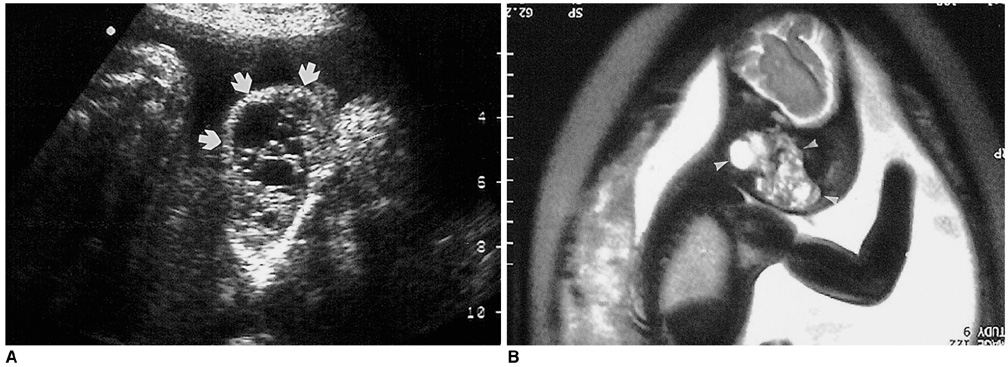
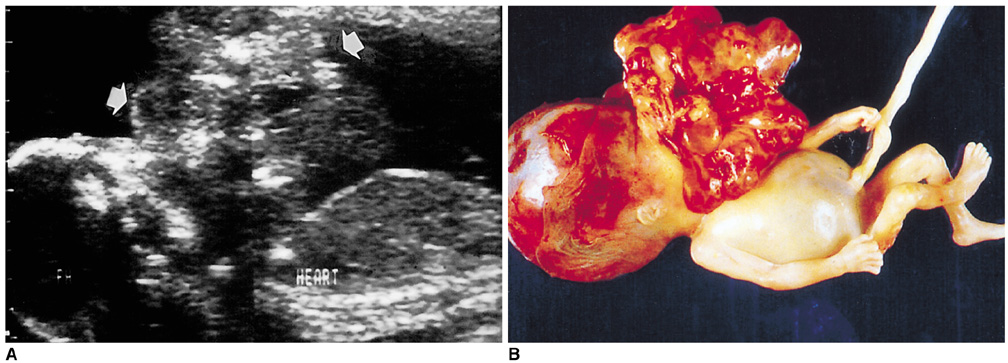
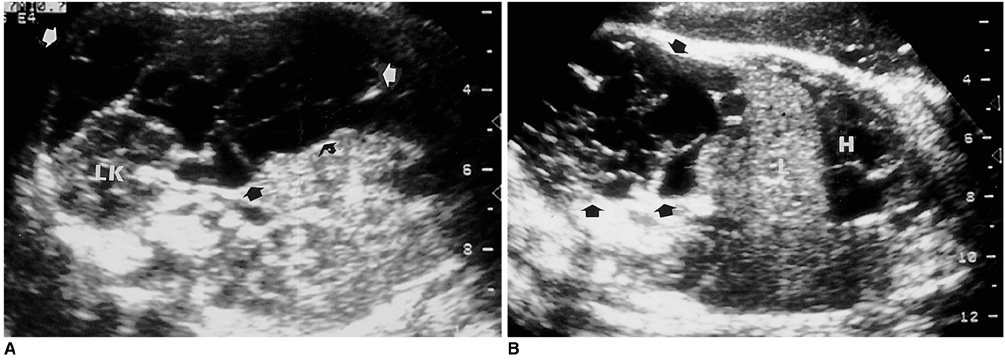
- A variety of neoplasms can develop in each tetal organ. Most fetal neoplasms can be detected by careful prenatal ultrasonographic examination. Some neoplosms show specific ultrasonographic findings suggesting the differential diagnosis, but others do not. Knowledge of the presence of a neoplasm in the fetus may alter the prenatal management of a pregnancy and the mode of delivery, and facilitates immediate postnatal treatment. During the last five years, we experienced 32 cases of fetal neoplasms in a variety of organs. We describe their typical ultrasonographic findings with correlating postnatal CT, MRI, and pathologic findings.
Keyword
MeSH Terms
Figure
Reference
-
1. Lipman SP, Pretorius DH, Rumack CM, et al. Fetal intracranial teratoma; US diagnosis of three cases and a review of the literature. Radiology. 1985. 157:491–494.2. Teal LN, Angtauco TL, Jimenez JF, Quirk JG. Fetal teratomas: antenatal diagnosis and clinical management. J Clin Ultrasound. 1988. 16:329–336.3. Buetow PC, Smirniotopoulos JG, Done S. Congenital brain tumors: a review of 45 cases. AJR. 1990. 155:587–593.4. Garaghty AV, Knott PD, Hanna HM. Prenatal diagnosis of fetal glioblastma multiforme. Prenat Diagn. 1989. 9:613–616.5. Sabet LM. Congenital glioblastoma multiforme associated with congestive heart failure. Arch Pathol Lab Med. 1982. 106:31–34.6. Zadvinskis DP, Benson MT, Kerr HH, et al. Congenital malformations of the cervicothoracic lymphatic system: embryology and pathogenesis. Radiographics. 1992. 12:1175–1189.7. Pui MH, Li ZP, Chen W, Chen JH. Lymphangioma: imaging diagnosis. Australasian Radiology. 1997. 41:324–328.8. Rempen A, Feige A. Differential diagnosis of sonographically detected tumors in the fetal cervical region. Europ J Obstet Gynecol Reprod Biol. 1985. 20:89–105.9. Kerner B, Flaum E, Mathews H, et al. Cervical teratoma: prenatal diagnosis and long-term follow-up. Prenat Diagn. 1998. 18:51–59.10. Rosenfeld CR, Coln CD, Duenhoelter JH. Fetal cervical teratoma as a cause of polyhydramnios. Pediatrics. 1979. 64:176–179.11. Holley D, Martin G, Brenner J, et al. Diagnosis and management of fetal cardiac tumors: A multicenter experience and review of published reports. J Am Coll Cardiol. 1995. 26:516–520.12. Giacoia GP. Fetal rhabdomyoma: a prenatal echocardiographic marker of tuberous sclerosis. Am J Perinatol. 1992. 9:111–114.13. Green KW, Bros-Koefoed R, Pollack P, et al. Antepartum diagnosis and management of multiple fetal cardiac tumors. J Ultrasound Med. 1991. 10:697–699.14. Takiff H, Calabria R, Yin L, Stabile BE. Mesenteric cysts and intra-abdominal cystic lymphangiomas. Arch Surg. 1985. 120:1266–1269.15. Stoupos C, Ros PR, Abbit PL, Burton SS, Gauger J. Bubbles in the belly: Imaging of cystic mesenteric or omental masses. Radiographics. 1994. 14:729–737.16. de Perrot M, Rostan O, Morel P, Le Coultre C. Abdominal lymphangioma in adults and children. Br J Surg. 1998. 85:395–397.17. Takano H, Smith WL. Gastrointestinal tumors of childhood. Radiol Clin North Am. 1997. 35:1367–1389.18. Chung KY, Mayo-Smith WW, Saini S, et al. Hepatocellular adenoma: MR imaging features with pathologic correlation. AJR. 1995. 165:303–308.19. Dreyfus M, Baldauf JJ, Dadoun K, Becmeur F, Berrut F, Ritter J. Prenatal diagnosis of hepatic hemangioma. Fetal Diagn Ther. 1996. 11:57–60.20. Chuileannain FN, Rowlands S, Sampson A. Ultrasonographic appearances of fetal hepatic hemangioma. J Ultrasound Med. 1999. 18:379–381.21. Fishman SJ, Mulliken JB. Hemangiomas and vascular malformations of infancy and childhood. Pediatr Clin North Am. 1993. 40(6):1177–1200.22. Irsutti M, Puget C, Baunin C, Duga I, Sarramon MF, Guitard J. Mesoblastic nephroma: prenatal ultrasonographic and MRI features. Pediatr Radiol. 2000. 30:147–150.23. Dimaggio HD, Farrell EE, Sholl J, et al. Congenital mesoblastic nephroma: prenatal ultrasonic findings and surgical excision in a very-low-birth-weight infant. J Clin Ultrasound. 1985. 13:506–508.24. Geirsson RT, Ricketts NE, Taylor DJ, et al. Prenatal appearance of a mesoblastic nephroma associated with polyhydroamnios. J Clin Ultrasound. 1985. 13:488–490.25. Bader JL, Miller RW. US cancer incidence and mortality in the first year of life. Am J Dis Child. 1979. 133:157–161.26. Ferraro EM, Fakhry J, Aruny J. Prenatal adrenal neuroblastoma: A case report with review of the literature. J Ultrasound Med. 1988. 7:275–278.27. Granata C, Fagnani AM, Gambini C, et al. Features and outcome of neuroblastoma detected before birth. J Pediatr Surg. 2000. 35:88–91.28. Sheth S, Nussbaum AR, Sanders RC, Hamper UM, Davison AJ. Prenatal diagnosis of sacrococcygeal teratoma: Sonographic-pathologic correlation. Radiology. 1988. 169:131–136.29. Tongsong T, Wanapirak C, Piyamongkol W, Sudasana J. Prenatal sonographic features of sacrococcygeal teratoma. Int J Gynaecol Obstet. 1999. 67:95–101.30. Bond SJ, Harrison MR, Schmidt KG, et al. Death due to high-output failure in fetal sacrococcygeal teratoma. J Pediatr Surg. 1990. 25:1287–1291.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Prenatal Ultrasonographic Diagnosis of Frequent Congenital Fetal Anomalies
- Prenatal Ultrasound of Horseshoe Kidney: A Case Report
- Recent Trends in Prenatal Diagnosis of Fetal Malformations
- Prenatal ultrasonography of craniofacial abnormalities
- Prenatal Detection of a Congenital Pancreatic Cyst by Ultrasound