Korean J Radiol.
2002 Mar;3(1):38-44. 10.3348/kjr.2002.3.1.38.
Sonographic Evaluation of Breast Nodules: Comparison of Conventional, Real-Time Compound, and Pulse-Inversion Harmonic Images
- Affiliations
-
- 1Department of Diagnostic Radiology, Korea University Hospital, Seoul, Korea. ssbk@dreamwiz.com
- 2Department of General Surgery, Korea University Hospital, Seoul, Korea.
- 3Department of Preventive Medicine, Korea University.
- 4Department of Diagnostic Radiology, Inje University Hospital.
- KMID: 1758445
- DOI: http://doi.org/10.3348/kjr.2002.3.1.38
Abstract
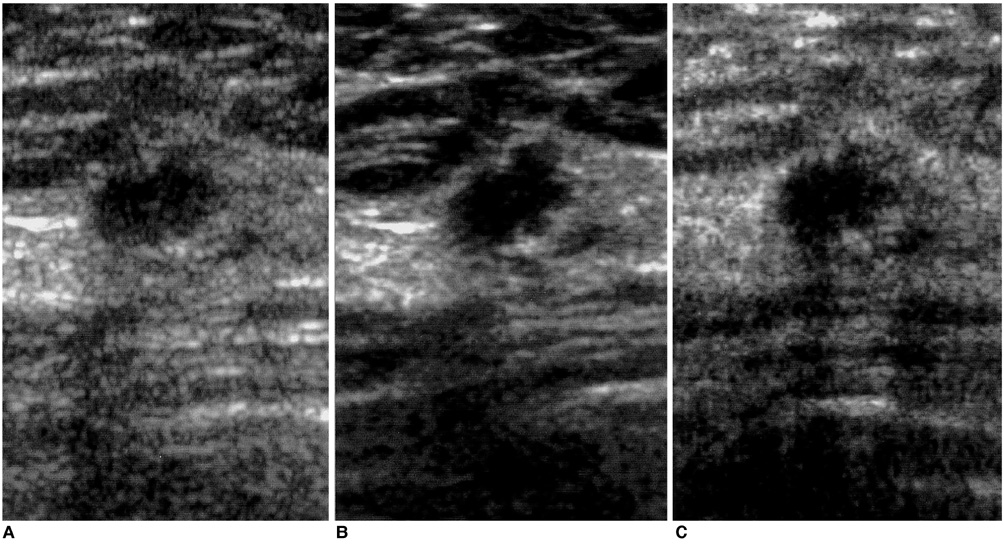
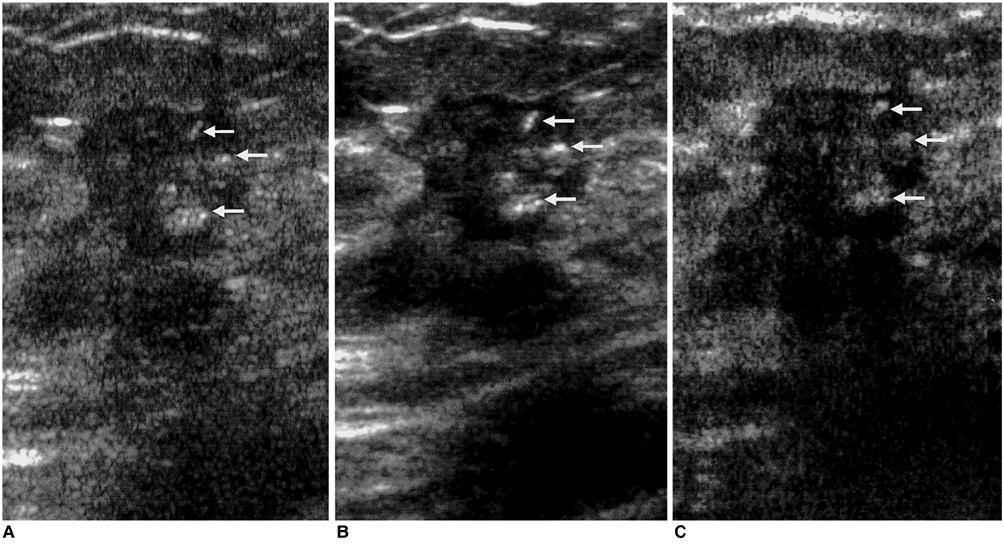
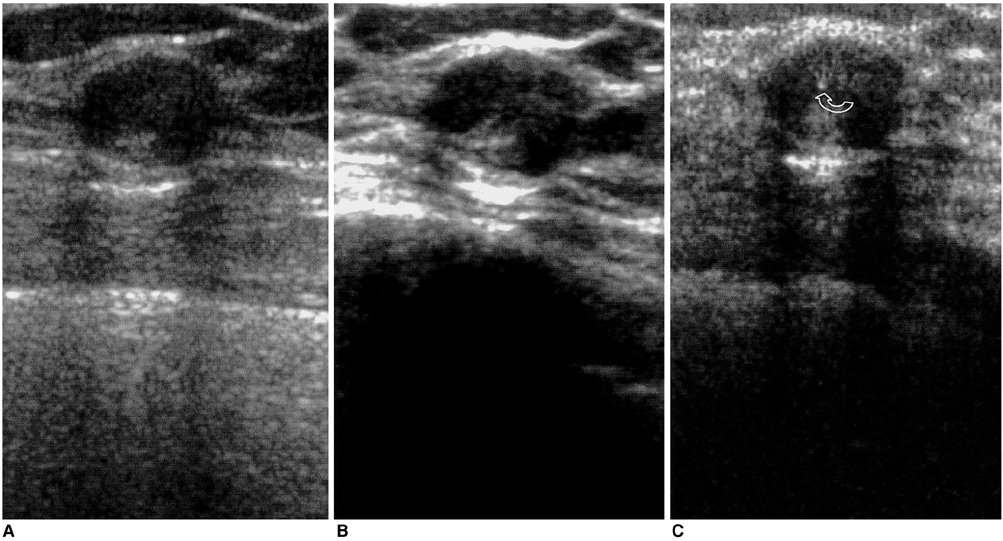
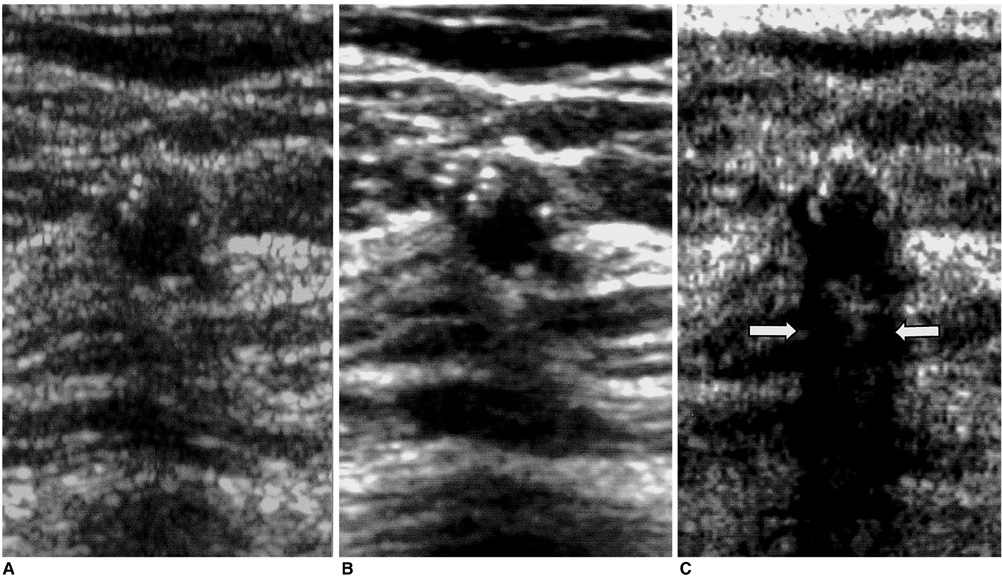
- OBJECTICE: To compare the use of conventional, real-time compound, and pulse-inversion harmonic imaging in the evaluation of breast nodules.
MATERIALS AND METHODS
Fifty-two breast nodules were included in this study, conducted between May and December 2000, in which conventional, real-time compound, and pulse-inversion harmonic images were obtained in the same plane. Three radiologists, each blinded to the interpretations of the other two, evaluated the findings, characterizing the lesions and ranking the three techniques from grade 1, the worst, to grade 3, the best. Lesion conspicuity was assessed, and lesions were also characterized in terms of their margin, clarity of internal echotexture, and clarity of posterior echo pattern. The three techniques were compared using Friedman's test, and interobserver agreement in image interpretation was assessed by means of the intraclass correlation coefficient.
RESULTS
With regard to lesion conspicuity, margin, and internal echotexture of the nodules, real-time compound imaging was the best technique (p < 0.05); in terms of posterior echo pattern, the best was pulse-inversion harmonic imaging (p < 0.05). Real-time compound and pulse inversion harmonic imaging were better than conventional sonography in all evaluative aspects. Interobserver agreement was greater than moderate.
CONCLUSION
Real-time compound and pulse-inversion harmonic imaging procedures are superior to conventional sonography in terms of both lesion conspicuity and the further characterization of breast nodules. Real-time compound imaging is the best technique for evaluation of the margin and internal echotexture of nodules, while pulse-inversion harmonic imaging is very effective for the evaluation of the posterior echo patterns.
Keyword
MeSH Terms
Figure
Reference
-
1. Hilton SW, Leopold GR, Olson LK, Wilson SA. Real-time breast sonography: application in 300 consecutive patients. AJR. 1986. 147:479–486.2. Cole-Beuglet C, Soriano RZ, Kurtz B, et al. Ultrasound analysis of 104 primary breast carcinomas classified according to histopathologic type. Radiology. 1983. 147:191–196.3. Cole-Beuglet C, Soriano RZ, Kurtz AB, Goldberg BB. Fibroadenoma of the breast: sonomammography correlated with pathology in 122 patients. AJR. 1983. 140:369–375.4. Jackson VP, Rothschild PA, Kreipke DL, et al. The spectrum of sonographic findings of fibroadenoma of the breast. Invest Radiol. 1986. 21:34–40.5. Heywang SH, Lipsit ER, Glassman LM, et al. Specificity of ultrasonography in the diagnosis of benign breast masses. J Ultrasound Med. 1984. 3:453–461.6. Jokich PM, Monticciolo DL, Adler YT. Breast ultrasonography. Radiol Clin North Am. 1992. 30:993–1009.7. Kopans DB, Meyer JE, Lindfors KK, Bucchianeri SS. Breast sonography to guide cyst aspiration and wire localization of occult solid lesions. AJR. 1984. 143:489–492.8. Kopans DB. Breast imaging and the standard of care for the symptomatic patient. Radiology. 1991. 187:608–611.9. Fornage BD, Sneige N, Faroux MJ, Andry E. Sonographic appearance and ultrasound guided fine-needle aspiration biopsy of breast carcinomas smaller than 1cm3. J Ultrasound Med. 1990. 9:559–560.10. Fornage BD, Lorigan JG, Andry E. Fibroadenoma of the breast: sonographic appearance. Radiology. 1989. 172:671–675.11. Harper PA, Kelly-Fry E, Noe JS, Bies RJ, Jackson VP. Ultrasound in the evaluation of solid breast masses. Radiology. 1983. 146:731–736.12. Kobayashi T. Diagnostic ultrasound in breast cancer: analysis of retrotumorous echo patterns correlated with sonic attenuation by cancerous connective tissue. J Clin Ultrasound. 1979. 7:471–479.13. Leucht WJ, Rabe DR, Humbert KD. Diagnostic value of different interpretative criteria in real-time sonography of the breast. Ultrasound Med Biol. 1988. 14:S 1. 59–73.14. Majewski A, Rosenthal H, Wagner HH. Results of real-time sonography and raster mammography of 200 breast cancers. ROFO Fortschr Nucleamed. 1986. 144:343–350.15. Smallwood JA, Guyer P, Dewbury K, Mengatti S, Royle GT, Taylor I. The accuracy of ultrasound in the diagnosis of breast disease. Ann R Coll Surg Engl. 1986. 68:19–22.16. Ueno E, Tohno E, Soeda S, et al. Dynamic tests in real-time breast echography. Ultrasound Med Biol. 1988. 14:S 1. 53–57.17. Stavros AT, Thickman D, Rapp CL, Dennis MA, Parker SH, Sisney GA. Solid breast nodules: use of sonography to distinguish between benign and malignant lesions. Radiology. 1995. 196:123–134.18. Shapiro RS, Wagreich J, Parsons RB, Stancato-Pasik A, Yeh HC, Lao R. Tissue harmonic imaging sonography: evaluation of image quality compared with conventional sonography. AJR. 1998. 171:1203–1206.19. Jang HJ, Lim HK, Lee WJ, et al. Ultrasonographic evaluation of focal hepatic lesions: comparison of pulse inversion harmonic, tissue harmonic, and conventional imaging techniques. J Ultrasound Med. 2000. 19:293–299.20. Kim BH, Lim HK, Choi MH, et al. Detection of parenchymal abnormalities in acute pyelonephritis by pulse inversion harmonic imaging with or without microbubble ultrasonographic contrast agent: correlation with computed tomography. J Ultrasound Med. 2001. 20:5–14.21. Shrout PE, Fleiss Jl. Intraclass correlations: used in assessing rater reliability. Psychol Bull. 1979. 86:420–428.22. Kim AY, Kim TK, Kim YH, Han JK, Choi BI. Comparison of harmonic and conventional power Doppler ultrasonography for the assessment of slow flow in hyperechoic tissue: experimental study using a Doppler phantom. Invest Radiol. 2000. 35:105–110.23. Burns PN, Wilson SR, Simpson DH. Pulse inversion imaging of liver blood flow: improved method for characterizing focal masses with microbubble contrast. Invest Radiol. 2000. 35:58–71.24. Carpenter DA, Dadd MJ, Kossoff FG. A multi-mode real-time scanner. Ultrasound Med Biol. 1980. 6:279–284.25. Berson M, Roncin A, Pourcelot L. Compound scanning with an electrically steered beam. Ultrasonic Imaging. 1981. 3:303–308.26. Jespersen SK, Wilhjelm JE, Sillesen H. Multi-angle compound imaging. Ultrasonic Imaging. 1998. 20:81–102.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison Study among Conventional, Tissue Harmonic and Pulse Inversion Harmonic Images to Evaluate Pleural Effusion and Ascites
- Value of Real-time Compound US in Diagnosis of Malignant Tumor in Breast Comparing with Conventional US, and Pulse Inversion Harmonic Images
- Ultrasonographic Evaluation of the Normal Kidney: Comparison of Fundamental, Tissue Harmonic, and Pulse Inversion Harmonic Imaging
- Does Real-time Compound Imaging Improve Evaluation of Breast Cancer Compared to Conventional Sonography?
- Ultrasound Evaluation of Normal and Abnormal Fetuses: Comparison of Conventional, Tissue Harmonic, and Pulse-Inversion Harmonic Imaging Techniques