J Korean Soc Radiol.
2013 Mar;68(3):251-255. 10.3348/jksr.2013.68.3.251.
MRI Findings of Juvenile Xanthogranuloma of the Spinal Cord: A Case Report
- Affiliations
-
- 1Department of Radiology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. parkhiji@gmail.com
- 2Department of Pathology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1748460
- DOI: http://doi.org/10.3348/jksr.2013.68.3.251
Abstract
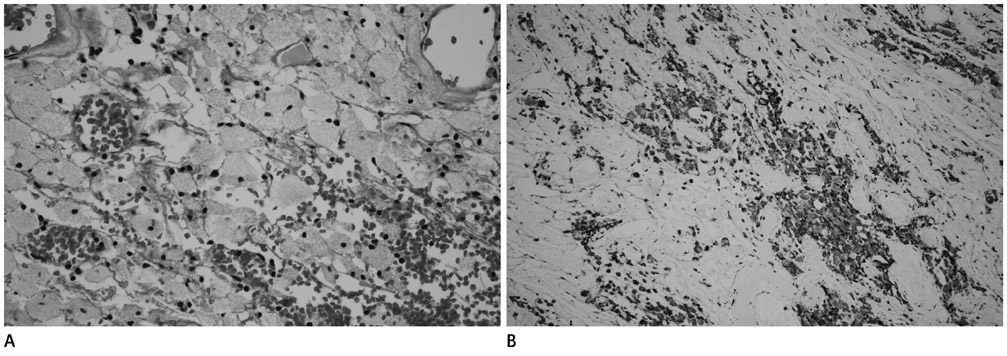
- Juvenile xanthogranuloma (JXG) is a proliferative histiocytic disorder experienced during childhood and adolescents. JXG commonly presents as a solitary cutaneous lesion. Despite the term "juvenile", development of the disease during adulthood is possible, although spinal JXG is extremely rare in adults. We describe a 67-year-old female patient who presented with an intradural-extramedullary (IDEM) tumor of the spinal cord. Magnetic resonance imaging (MRI) findings indicative of JXG of the spinal cord were seen, which was then confirmed pathologically. A lumbar spinal MRI with contrast enhancement showed an oval-shaped, well-defined IDEM tumor at the L1 level. This tumor had mixed signal intensity on the T1-weighted image and high signal intensity on the T2-weighted image. Central homogenous enhancement was observed after contrast administration.
MeSH Terms
Figure
Reference
-
1. Dehner LP. Juvenile xanthogranulomas in the first two decades of life: a clinicopathologic study of 174 cases with cutaneous and extracutaneous manifestations. Am J Surg Pathol. 2003. 27:579–593.2. Inoue H, Seichi A, Yamamuro K, Kojima M, Kimura A, Hoshino Y. Dumbbell-type juvenile xanthogranuloma in the cervical spine of an adult. Eur Spine J. 2011. 20:Suppl 2. S343–S347.3. Iwasaki Y, Hida K, Nagashima K. Cauda equina xanthogranulomatosis. Br J Neurosurg. 2001. 15:72–73.4. Lee SJ, Jo DJ, Lee SH, Kim SM. Solitary xanthogranuloma of the upper cervical spine in a male adult. J Korean Neurosurg Soc. 2012. 51:54–58.5. Ayres WW, Haymaker W. Xanthoma and cholesterol granuloma of the choroid plexus. Report of the pathological aspects in 29 cases. J Neuropathol Exp Neurol. 1960. 19:280–295.6. Hernandez-Martin A, Baselga E, Drolet BA, Esterly NB. Juvenile xanthogranuloma. J Am Acad Dermatol. 1997. 36(3 Pt 1):355–367. quiz 368-369.7. Freyer DR, Kennedy R, Bostrom BC, Kohut G, Dehner LP. Juvenile xanthogranuloma: forms of systemic disease and their clinical implications. J Pediatr. 1996. 129:227–237.8. Rampini PM, Alimehmeti RH, Egidi MG, Zavanone ML, Bauer D, Fossali E, et al. Isolated cervical juvenile xanthogranuloma in childhood. Spine (Phila Pa 1976). 2001. 26:1392–1395.9. Yuh EL, Barkovich AJ, Gupta N. Imaging of ependymomas: MRI and CT. Childs Nerv Syst. 2009. 25:1203–1213.10. Lin YZ, Zhang XL. [Diagnosis of intramedullary spinal cord ependymomas and astrocytomas using magnetic resonance imaging: analysis of 15 cases]. Di Yi Jun Yi Da Xue Xue Bao. 2004. 24:847–848.