J Korean Soc Radiol.
2013 Mar;68(3):197-200. 10.3348/jksr.2013.68.3.197.
Relapsing and Progressive Tumefactive Demyelinating Form of Central Nervous System Involvement in a Patient with Progressive Systemic Sclerosis
- Affiliations
-
- 1Department of Radiology, Catholic University of Daegu School of Medicine, Daegu, Korea.
- 2Department of Radiology, Kyungpook National University Hospital, Daegu, Korea. leehuijoong@knu.ac.kr
- KMID: 1748450
- DOI: http://doi.org/10.3348/jksr.2013.68.3.197
Abstract
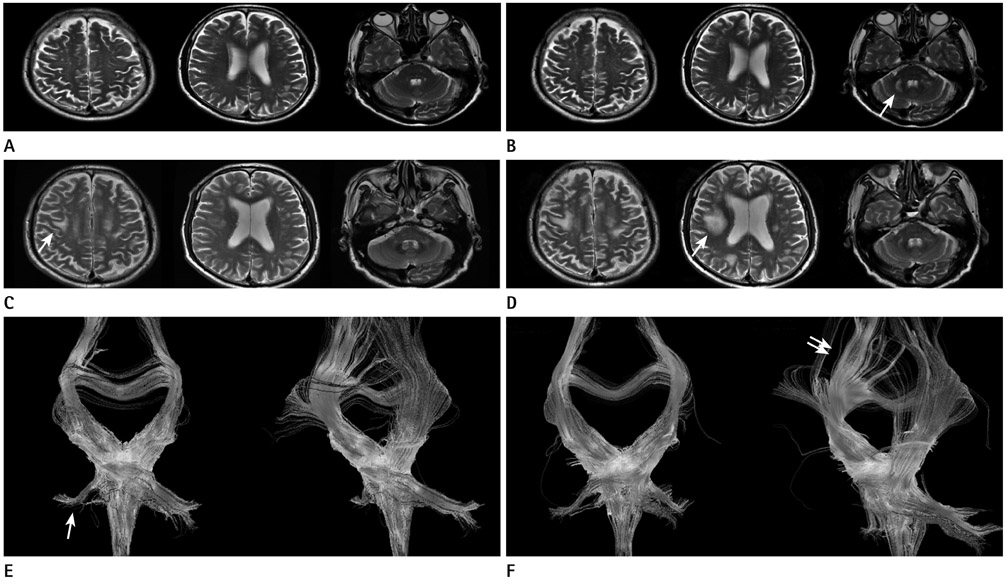
- White matter hyper intensities (WMHI) on MRI are not rare in patients with progressive systemic sclerosis (PSS). In this presentation, WMHI were developed in both middle cerebellar peduncles and temporal white matter in a patient with PSS, and regressed after medication of high dose steroid. However, new lesions were developed in the subcortices of both precentral gyri, and progressed rapidly to tumefactive hyperintensity on MRI. We report an unusual relapsing and progressive tumefactive demyelinating form of central nervous system involvement in PSS.
Figure
Reference
-
1. Lucivero V, Mezzapesa DM, Petruzzellis M, Carella A, Lamberti P, Federico F. Ischaemic stroke in progressive systemic sclerosis. Neurol Sci. 2004. 25:230–233.2. Mohammed RH, Sabry YY, Nasef AA. Brain MRI screening showing evidences of early central nervous system involvement in patients with systemic sclerosis. Rheumatol Int. 2011. 31:667–671.3. Sardanelli F, Iozzelli A, Cotticelli B, Losacco C, Cutolo M, Sulli A, et al. White matter hyperintensities on brain magnetic resonance in systemic sclerosis. Ann Rheum Dis. 2005. 64:777–779.4. Kanzato N, Matsuzaki T, Komine Y, Saito M, Saito A, Yoshio T, et al. Localized scleroderma associated with progressing ischemic stroke. J Neurol Sci. 1999. 163:86–89.5. Simeoni S, Puccetti A, Tinazzi E, Tomelleri G, Corrocher R, Lunardi C. Systemic sclerosis and superficial siderosis of the central nervous system: casuality or causality? Rheumatol Int. 2008. 28:815–818.6. Nobili F, Cutolo M, Sulli A, Castaldi A, Sardanelli F, Accardo S, et al. Impaired quantitative cerebral blood flow in scleroderma patients. J Neurol Sci. 1997. 152:63–71.7. Chung MH, Sum J, Morrell MJ, Horoupian DS. Intracerebral involvement in scleroderma en coup de sabre: report of a case with neuropathologic findings. Ann Neurol. 1995. 37:679–681.8. Stone J, Franks AJ, Guthrie JA, Johnson MH. Scleroderma "en coup de sabre": pathological evidence of intracerebral inflammation. J Neurol Neurosurg Psychiatry. 2001. 70:382–385.9. Pathak R, Gabor AJ. Scleroderma and central nervous system vasculitis. Stroke. 1991. 22:410–413.10. Torabi AM, Patel RK, Wolfe GI, Hughes CS, Mendelsohn DB, Trivedi JR. Transverse myelitis in systemic sclerosis. Arch Neurol. 2004. 61:126–128.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Multiple Sclerosis Presenting as Acute Disseminated Encephalomyelitis
- Two Cases of Primary Sjogren's Syndrome Presenting as Relapsing-Remitting Multiple Sclerosis
- A Tumefactive Multiple Sclerosis Lesion in the Brain: An Uncommon Site with Atypical Magnetic Resonance Image Findings
- A Case of Multiple Sclerosis with Isolated Vertigo
- A Case of Overlap Syndrome of Systemic Sclerosis and Cryoglobulinemic Vasculitis With Central Nervous System Involvement