Initial Experience Using the 5MAX(TM) ACE Reperfusion Catheter in Intra-arterial Therapy for Acute Ischemic Stroke
- Affiliations
-
- 1Cerebrovascular Center, Cleveland Clinic, Cleveland, OH, United States. huif@ccf.org
- KMID: 1738340
- DOI: http://doi.org/10.7461/jcen.2014.16.4.350
Abstract
OBJECTIVES
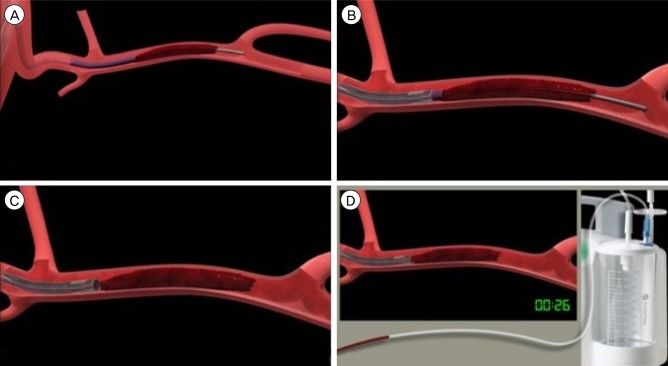
The 5MAX ACE is a new large bore aspiration catheter available for vessel recanalization for treatment of acute ischemic stroke (AIS). We report our initial experience with its use.
METHODS
A retrospective analysis of patients undergoing intra-arterial therapy for AIS using the 5MAX ACE reperfusion catheter at our institution was performed. Patient demographics, clinical characteristics and procedural data were obtained from chart review. Successful recanlization was defined as achievement of Thrombolysis in Cerebral Infarction score (TICI) 2b-3 and time to recanalization was defined as time from groin puncture to achievement of at least TICI 2b recanalization.
RESULTS
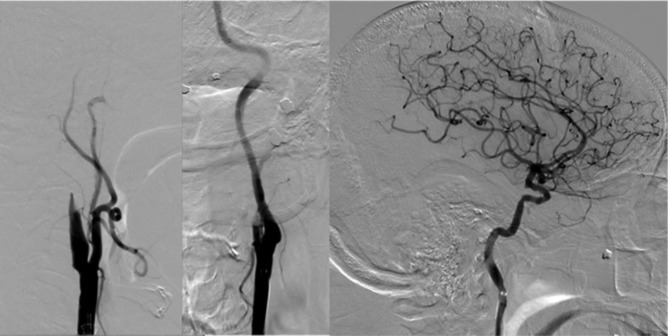
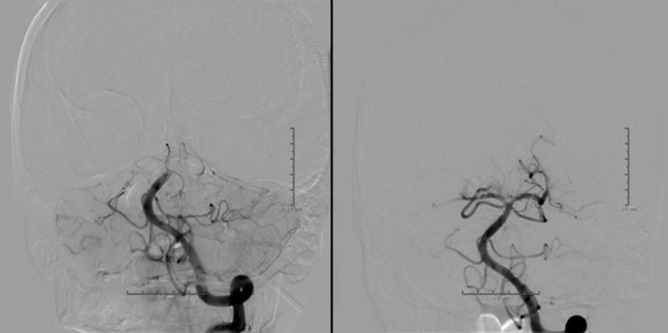
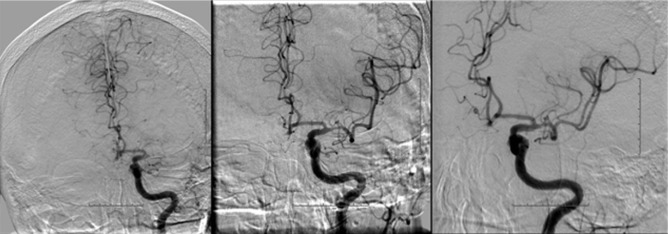
The 5MAX ACE was used in 15 patients from July-October 2013. Direct aspiration was used as the primary technique in 10/15 (67%) patients. Out of these, aspiration alone was sufficient for recanalization in 3 (20%) patients. In the remaining 7 (47%) patients, additional devices were used. In 5/15 (33%) patients, combined aspiration/stentriever thrombectomy using Solitaire(TM) (3/5 patients) and Penumbra 3D Separator(TM) (2/5 patients) were used as the primary technique. Successful recanlization (TICI 2b-3) was achieved in 11/15 (73%) patients. Average time from groin puncture to successful recanalization was 46 +/- 30 minutes (range 14-98 minutes). There were no procedural complications.
CONCLUSION
The 5MAX ACE is a useful recanalization tool, either by direct aspiration or combined stentriever/aspiration. It may be most advantageous with large clots in the internal carotid artery. The potential for effective and faster recanalization using this device alone or in combination may be a good topic for future study.
MeSH Terms
Figure
Cited by 4 articles
-
Pseudoaneurysm Formation after Repetitive Suction Thrombectomy Using a Penumbra Suction Catheter
Eun-Oh Jeong, Hyon-Jo Kwon, Seung-Won Choi, Hyeon-Song Koh
J Cerebrovasc Endovasc Neurosurg. 2016;18(3):296-301. doi: 10.7461/jcen.2016.18.3.296.Dual Mechanical Thrombectomy for Recanalization of a Resistant Acute Posterior Circulation Stroke
Ahmet Peker, Ayça Akgoz, Ethem Murat Arsava, Mehmet Akif Topçuoglu, Anil Arat
J Cerebrovasc Endovasc Neurosurg. 2017;19(2):96-100. doi: 10.7461/jcen.2017.19.2.96.Initial Experience of ACE68 Reperfusion Catheter in Patients with Acute Ischemic Stroke Related to Internal Carotid Artery Occlusion
Hyoung-Gyu Jang, Jung-Soo Park, Jong-Myong Lee, Hyo-Sung Kwak
J Korean Neurosurg Soc. 2019;62(5):545-550. doi: 10.3340/jkns.2019.0108.Forced suction thrombectomy in patients with acute ischemic stroke using the SOFIA Plus device
Hyun Ki Roh, Min-Wook Ju, Hyoung Soo Byoun, Bumsoo Park, Kwang Hyon Park, Jeongwook Lim
J Cerebrovasc Endovasc Neurosurg. 2022;24(3):241-248. doi: 10.7461/jcen.2022.E2021.12.002.
Reference
-
1. Broderick JP, Palesch YY, Demchuk AM, Yeatts SD, Khatri P, Hill MD, et al. Interventional Management of Stroke (IMS) III Investigators. Endovascular therapy after intravenous t-PA versus t-PA alone for stroke. N Engl J Med. 2013; 3. 368(10):893–903. PMID: 23390923.2. Dumont TM, Mokin M, Sorkin GC, Levy EI, Siddiqui AH. Aspiration thrombectomy in concert with stent thrombectomy. J Neurointerv Surg. 2014; 5. 6(4):e26. PMID: 23868216.
Article3. Frei D, Gerber J, Turk A, McPherson M, Heck D, Hui F, et al. The SPEED study: initial clinical evaluation of the Penumbra novel 054 Reperfusion Catheter. J Neurointerv Surg. 2013; 5. 5(Suppl 1):i74–i76. PMID: 23299104.
Article4. Kang DH, Hwang YH, Kim YS, Park J, Kwon O, Jung C. Direct Thrombus Retrieval Using the Reperfusion Catheter of the Penumbra System: Forced-Suction Thrombectomy in Acute Ischemic Stroke. AJNR Am J Neuroradiol. 2011; 2. 32(2):283–287. PMID: 21087940.
Article5. Nogueira RG, Lutsep HL, Gupta R, Jovin TG, Albers GW, Walker GA, et al. Trevo versus Merci retrievers for thrombectomy revascularisation of large vessel occlusions in acute ischaemic stroke (TREVO 2): a randomised trial. Lancet. 2012; 10. 380(9849):1231–1240. PMID: 22932714.
Article6. Saver JL, Jahan R, Levy EI, Jovin TG, Baxter B, Nogueira RG, et al. Solitaire flow restoration device versus the Merci retriever in patients with acute ischaemic stroke (SWIFT): a randomised, parallel-group, non-inferiority trial. Lancet. 2012; 10. 380(9849):1241–1249. PMID: 22932715.
Article7. Penumbra Pivotal Stroke Trial Investigators. The penumbra pivotal stroke trial: Safety and effectiveness of a new generation of mechanical devices for clot removal in intracranial large vessel occlusive disease. Stroke. 2009; 8. 40(8):2761–2768. PMID: 19590057.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Thrombectomy in Acute Ischemic Stroke: Challenges to Procedural Success
- Thrombolytic Treatment of Acute Stroke
- Forced Arterial Suction Thrombectomy Using Distal Access Catheter in Acute Ischemic Stroke
- Recent advances in thrombolysis of acute ischemic stroke
- Life-Threatening Anaphylactoid Reaction in an Acute Ischemic Stroke Patient With Intravenous rt-PA Thrombolysis, Followed by Successful Intra-Arterial Thrombolysis