Korean J Lab Med.
2011 Jul;31(3):157-161. 10.3343/kjlm.2011.31.3.157.
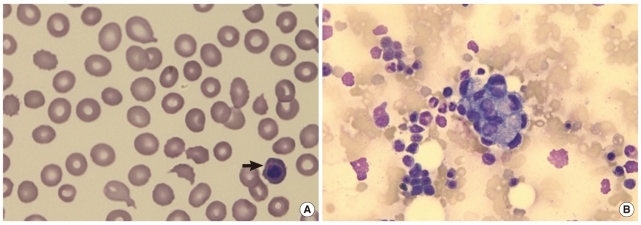
Microangiopathic Hemolytic Anemia as the First Manifestation of Metastatic Signet Ring Cell Carcinoma of Unknown Origin: A Case Report and Review of Literature
- Affiliations
-
- 1Department of Laboratory Medicine, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea. drwhy@hanmail.net
- 2Department of Pathology, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 1735847
- DOI: http://doi.org/10.3343/kjlm.2011.31.3.157
Abstract
- Microangiopathic hemolytic anemia (MAHA) occurs occasionally as a paraneoplastic syndrome in some solid tumors, but MAHA accompanied by signet ring cell carcinoma of an unknown origin is very rare. In this study, we present the case of an 80-yr-old man who was admitted to the hospital because of a 1-month history of lower back pain and dyspnea. He was diagnosed with MAHA on the basis of the laboratory findings that revealed anemia with schistocytes, decreased haptoglobin levels, and a negative direct Coombs' test. Bone marrow examination, which was performed because of the progression of anemia, revealed bone marrow metastases of signet ring cell carcinoma with extensive bone marrow necrosis. However, the primary origin of this signet ring cell carcinoma was not found. When the cause of progressive MAHA is unknown, the possibility of cancer-associated MAHA must be excluded by performing additional tumor workup, including the detection of tumor markers, gastric and colorectal endoscopic examinations, bone marrow examinations, and positron emission tomography-computed tomography or bone scans.
MeSH Terms
-
Aged, 80 and over
Bone Marrow Neoplasms/complications/*diagnosis/pathology
Carcinoma, Signet Ring Cell/complications/*diagnosis/pathology
Endoscopy, Gastrointestinal
Haptoglobins/metabolism
Humans
Immunohistochemistry
Male
Necrosis/etiology
Neoplasm Metastasis
Positron-Emission Tomography
Purpura, Thrombotic Thrombocytopenic/*diagnosis/etiology
Tomography, X-Ray Computed
Tumor Markers, Biological/analysis
Figure
Reference
-
1. Brain MC, Dacie JV, Hourihane DO. Microangiopathic haemolytic anaemia: the possible role of vascular lesions in pathogenesis. Br J Haematol. 1962; 8:358–374. PMID: 14014893.
Article2. Elliott MA, Letendre L, Gastineau DA, Winters JL, Pruthi RK, Heit JA. Cancer-associated microangiopathic hemolytic anemia with thrombocytopenia: an important diagnostic consideration. Eur J Haematol. 2010; 85:43–50. PMID: 20331741.
Article3. Lee JL, Lee JH, Kim MK, Cho HS, Bae YK, Cho KH, et al. A case of bone marrow necrosis with thrombotic thrombocytopenic purpura as a manifestation of occult colon cancer. Jpn J Clin Oncol. 2004; 34:476–480. PMID: 15371467.
Article4. Kim YJ, Choi HM, Jung BG, Lee CK, Chung SY. Two cases of microangiopathic hemolytic anemia in patients with gastric cancer. Korean J Hematol. 1990; 25:575–579.5. Suh HC, Min YH, Kang WC, Lee S, Chong SY, Hahn JS, et al. A case of bone marrow metastatic malignant melanoma presenting microangiopathic hemolytic anemia as initial clinical findings. Korean J Hematol. 1996; 31:457–464.6. Youk DW, Choi MK, Kim KH, Kim HK, Park CW, Kim BK, et al. Microangiopathic homolytic anemia in patients with gastrointestinal malignancy. Korean J Hematol. 1983; 18:207–214.7. Lee MA, Shim SI. A review of ten cases of microangiopathic hemolytic anemia. Korean J Clin Pathol. 1994; 14:43–48.8. Arkenau HT, Müssig O, Buhr T, Jend HH, Porschen R. Microangiopathic hemolytic anemia (MAHA) as paraneoplastic syndrome in metastasized signet ring cell carcinomas: case reports and review of the literature. Z Gastroenterol. 2005; 43:719–722. PMID: 16088769.9. Abdel Samie A, Sandritter B, Theilmann L. Severe microangiopathic hemolytic anemia as first manifestation of a CUP syndrome. Rapid hematologic remission under polychemotherapy. Med Klin (Munich). 2004; 99:148–153. PMID: 15024487.10. Hahn JS, Lee DH, Lee SJ, Min YH, Ko YW. A clinical study on microangiopathic hemolytic anemia. Korean J Hematol. 1991; 26:263–279.11. Etoh T, Baba H, Taketomi A, Nakashima H, Kohnoe S, Seo Y, et al. Diffuse bone metastasis with hematologic disorders from gastric cancer: clinicopathological features and prognosis. Oncol Rep. 1999; 6:601–605. PMID: 10203599.
Article12. Francis KK, Kalyanam N, Terrell DR, Vesely SK, George JN. Disseminated malignancy misdiagnosed as thrombotic thrombocytopenic purpura: A report of 10 patients and a systematic review of published cases. Oncologist. 2007; 12:11–19. PMID: 17227897.
Article13. Oberic L, Buffet M, Schwarzinger M, Veyradier A, Clabault K, Malot S, et al. Cancer awareness in atypical thrombotic microangiopathies. Oncologist. 2009; 14:769–779. PMID: 19684072.
Article14. Hilgard P, Gordon-Smith EC. Microangiopathic haemolytic anaemia and experimental tumour-cell emboli. Br J Haematol. 1974; 26:651–659. PMID: 4845651.
Article15. Murgo AJ. Thrombotic microangiopathy in the cancer patient including those induced by chemotherapeutic agents. Semin Hematol. 1987; 24:161–177. PMID: 3310241.16. Caine GJ, Stonelake PS, Lip GY, Kehoe ST. The hypercoagulable state of malignancy: pathogenesis and current debate. Neoplasia. 2002; 4:465–473. PMID: 12407439.
Article17. Antonioli DA, Goldman H. Changes in the location and type of gastric adenocarcinoma. Cancer. 1982; 50:775–781. PMID: 7093911.
Article18. Connelly JH, Robey-Cafferty SS, el-Naggar AK, Cleary KR. Exophytic signet-ring cell carcinoma of the colorectum. Arch Pathol Lab Med. 1991; 115:134–136. PMID: 1847034.19. Kim KS, Kim YD, Han KH, Lee SH, Kim JH, Choi HY, et al. Endoscopic findings and clinicopathological characteristics of signet ring cell carcinoma of the stomach. Korean J Med. 2007; 73:596–602.20. Saito S, Iwaki H. Mucin-producing carcinoma of the prostate: review of 88 cases. Urology. 1999; 54:141–144. PMID: 10414741.
Article21. Sung CO, Seo JW, Kim KM, Do IG, Kim SW, Park CK. Clinical significance of signet-ring cells in colorectal mucinous adenocarcinoma. Mod Pathol. 2008; 21:1533–1541. PMID: 18849918.
Article22. Yokota T, Kunii Y, Teshima S, Yamada Y, Saito T, Kikuchi S, et al. Signet ring cell carcinoma of the stomach: a clinicopathological comparison with the other histological types. Tohoku J Exp Med. 1998; 186:121–130. PMID: 10223615.
Article23. Akamatsu S, Takahashi A, Ito M, Ogura K. Primary signet-ring cell carcinoma of the urinary bladder. Urology. 2010; 75:615–618. PMID: 19819534.
Article24. Tot T. Cytokeratins 20 and 7 as biomarkers: usefulness in discriminating primary from metastatic adenocarcinoma. Eur J Cancer. 2002; 38:758–763. PMID: 11937308.25. Nies BA, Kundel DW, Thomas LB, Freireich EJ. Leukopenia, bone pain, and bone necrosis in patients with acute leukemia: a clinicopathologic complex. Ann Intern Med. 1965; 62:698–705. PMID: 14274834.26. Janssens AM, Offner FC, Van Hove WZ. Bone marrow necrosis. Cancer. 2000; 88:1769–1780. PMID: 10760751.
Article27. Hahn JS, Lee HL, Lee SJ, Min YH, Ko YW, Yang WI. A clinical study on bone marrow necrosis. Korean J Hematol. 1991; 26:135–149.28. Jeong GY, Yoon HR, Kim SH. A case of bone marrow necrosis preceeding acute monoblastic leukemia. Korean J Clin Pathol. 1999; 19:172–176.29. Kaidar-Person O, Nasrallah H, Haim N, Dann EJ, Bar-Sela G. Disseminated carcinoma diagnosed by bone marrow biopsy in patients with microangiopathic hemolytic anemia and thrombocytopenia: a report of two cases with gastric cancer and a review of the literature. J Gastrointest Cancer. 2010; in press.
Article30. Ozkalemkas F, Ali R, Ozkocaman V, Ozcelik T, Ozan U, Ozturk H, et al. The bone marrow aspirate and biopsy in the diagnosis of unsuspected nonhematologic malignancy: a clinical study of 19 cases. BMC Cancer. 2005; 5:144. PMID: 16262899.
Article31. Kadikoylu G, Barutca S, Tataroglu C, Kafkas S, Erpek H, Meydan N, et al. Thrombotic thrombocytopenic purpura as the first manifestation of metastatic adenocarcinoma in a young woman. Transfus Apher Sci. 2010; 42:39–42. PMID: 19926523.
Article32. Tsuchiya Y, Ishibashi H, Ohtsuka T, Nagasawa K, Niho Y, Ide K. Mucin-producing signet ring cell carcinoma of stomach accompanied by microangiopathic hemolytic anemia and disseminated intravascular coagulation: a case report. Fukuoka Igaku Zasshi. 1989; 80:477–481. PMID: 2559010.33. Abdel Samie A, Sandritter B, Theilmann L. Severe microangiopathic hemolytic anemia as first manifestation of a CUP syndrome. Rapid hematologic remission under polychemotherapy. Med Klin (Munich). 2004; 99:148–153. PMID: 15024487.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cytologic Features of Signet Ring Cell Carcinoma of the Uterine Cervix: A Report of Two Cases
- Radiologic findings of metastatic signet ring cell carcinoma to the breast from stomach
- A Case of Primary Signet Ring Cell Carcinoma of the Uterine Cervix
- Signet Ring Cell Carcinoma of the Prostate A report of two cases
- Primary Signet Ring Cell Adenocarcinoma of the Prostate