Yonsei Med J.
2005 Apr;46(2):300-304. 10.3349/ymj.2005.46.2.300.
Optic Nerve Injury Secondary to Endoscopic Sinus Surgery: an Analysis of Three Cases
- Affiliations
-
- 1Department of Otorhinolaryngology, Yonsei University College of Medicine, Seoul, Korea. jhyoon@yumc.yonsei.ac.kr
- 2Department of Otorhinolaryngology, Ajou University College of Medicine, Suwon, Korea.
- 3The Brain Korea 21 Project for Medical Sciences, Korea.
- KMID: 1734060
- DOI: http://doi.org/10.3349/ymj.2005.46.2.300
Abstract
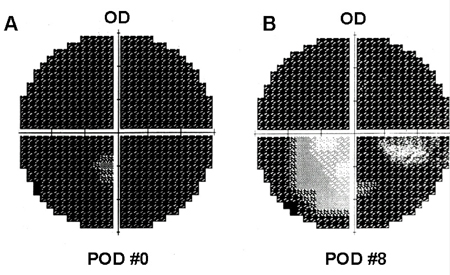
- Major orbital complications after the endoscopic sinus surgeries are rare and of these, optic nerve injury is one of the most serious. This study was to undertaken to analyze 3 cases of optic nerve injury after endoscopic sinus surgery. The three cases included one patient with a loss of visual acuity and visual field defect, and two patients with total blindness. In all cases, no improvement of visual acuity was observed despite treatment. It is important to frequently check the location and direction of the endoscope during surgery to avoid optic nerve injury. In addition, surgeons must have a precise knowledge of the detailed anatomy through cadaver dissections, an ability to interpret the PNS CT scan and experienced procedural surgical skills.
MeSH Terms
Figure
Reference
-
1. Kennedy DW, Senior BA. Endoscopic sinus surgery: a review. Otolaryngol Clin North Am. 1997. 30:313–330.2. Rene C, Rose GE, Lenthall R, et al. Major orbital complications of endoscopic sinus surgery. Br J Ophthalmol. 2001. 85:598–603.3. Driben JS, Bolger WE, Robles HA, Cable B, Zinreich J. The Reliability of Computerized Tomographic Detection of the Onodi (sphenoethmoid) Cell. Am J Rhinol. 1998. 12:105–111.4. Yeoh KH, Tan KK. The optic nerve in the posterior ethmoid in Asians. Acta Otolaryngol (Stockh). 1994. 114:329–336.5. Newell F. Ophthalmology. 1969. St. Louis: The CV Mosby Company;26–27.6. Rootman J, Stewart B, Goldberg RA. Orbital surgery. 1995. Philadelphia: Lippincott;79–146.7. Hayreh SS, Dass R. The ophthalmic artery. II: Ontraorbital course. Br J Ophthalmol. 1962. 46:165–185.8. Hayreh SS. The ophthalmic artery. III: Branches. Br J Ophthalmol. 1962. 46:212–247.9. Stankiewiez JA. Blindness and Intranansal Endoscopic Ethmoidectomy: Prevention and management. Otolaryngol Head Neck Surg. 1989. 101:320–329.10. Buus DR, Tse DT, Farris BK. Ophthalmic complications of sinus surgery. Ophthalmology. 1990. 97:612–619.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Delayed Ischemic Optic Neuropathy after Endoscopic Sinus Surgery: A Case Report
- A Case of Medial Rectus Muscle Injury and Optic Nerve Transection Developed During Functional Endoscopic Sinus Surgery
- A Case of Optic Nerve Decompression in a Patient with Retrobulbar Neuritis Secondary to Paranasal Sinusitis
- A Case of Optic Neuritis Secondary to Fungal Sphenoid Sinusitis
- A Case of Fungal Sphenoid Sinusitis with Visual Loss