Korean J Radiol.
2014 Aug;15(4):443-447. 10.3348/kjr.2014.15.4.443.
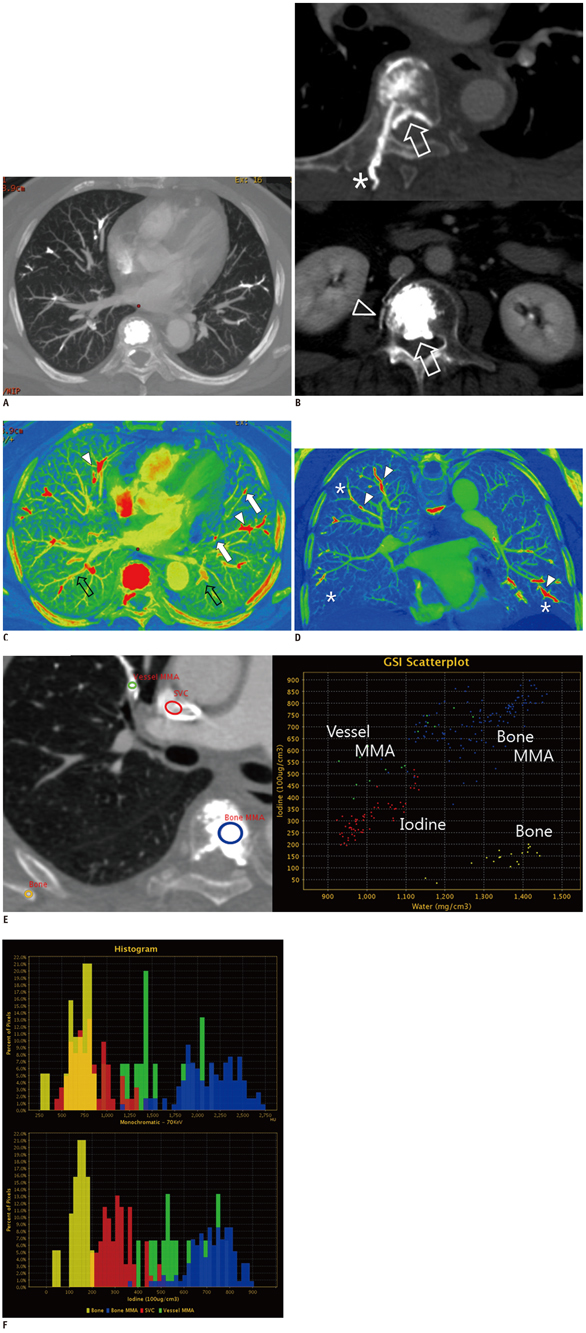
Pulmonary Bone Cement Embolism: CT Angiographic Evaluation with Material Decomposition Using Gemstone Spectral Imaging
- Affiliations
-
- 1Department of Radiology, Soonchunhyang University Hospital Bucheon, Bucheon 420-767, Korea. acarad@naver.com
- KMID: 1731047
- DOI: http://doi.org/10.3348/kjr.2014.15.4.443
Abstract
- We report a case of pulmonary bone cement embolism in a female who presented with dyspnea following multiple sessions of vertebroplasty. She underwent spectral CT pulmonary angiography and the diagnosis was made based on enhanced visualization of radiopaque cement material in the pulmonary arteries and a corresponding decrease in the parenchymal iodine content. Here, we describe the CT angiography findings of bone cement embolism with special emphasis on the potential benefits of spectral imaging, providing additional information on the material composition.
MeSH Terms
Figure
Reference
-
1. Galibert P, Deramond H, Rosat P, Le Gars D. [Preliminary note on the treatment of vertebral angioma by percutaneous acrylic vertebroplasty]. Neurochirurgie. 1987; 33:166–168.2. Krueger A, Bliemel C, Zettl R, Ruchholtz S. Management of pulmonary cement embolism after percutaneous vertebroplasty and kyphoplasty: a systematic review of the literature. Eur Spine J. 2009; 18:1257–1265.3. Barragán-Campos HM, Vallée JN, Lo D, Cormier E, Jean B, Rose M, et al. Percutaneous vertebroplasty for spinal metastases: complications. Radiology. 2006; 238:354–362.4. Choe DH, Marom EM, Ahrar K, Truong MT, Madewell JE. Pulmonary embolism of polymethyl methacrylate during percutaneous vertebroplasty and kyphoplasty. AJR Am J Roentgenol. 2004; 183:1097–1102.5. Remy-Jardin M, Pistolesi M, Goodman LR, Gefter WB, Gottschalk A, Mayo JR, et al. Management of suspected acute pulmonary embolism in the era of CT angiography: a statement from the Fleischner Society. Radiology. 2007; 245:315–329.6. Lu GM, Wu SY, Yeh BM, Zhang LJ. Dual-energy computed tomography in pulmonary embolism. Br J Radiol. 2010; 83:707–718.7. Lu GM, Zhao Y, Zhang LJ, Schoepf UJ. Dual-energy CT of the lung. AJR Am J Roentgenol. 2012; 199:5 Suppl. S40–S53.8. Sun YS, Zhang XY, Cui Y, Tang L, Li XT, Chen Y, et al. Spectral CT imaging as a new quantitative tool? Assessment of perfusion defects of pulmonary parenchyma in patients with lung cancer. Chin J Cancer Res. 2013; 25:722–728.9. Ghaye B. Peripheral pulmonary embolism on multidetector CT pulmonary angiography. JBR-BTR. 2007; 90:100–108.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Asymptomatic Bone Cement Pulmonary Embolism after Percutaneous Vertebroplasty: A Case Report
- Pulmonary Bone Cement Embolism Following Percutaneous Vertebroplasty
- Transcatheter Removal of Bone Cement Embolism in the Right Atrium after Percutaneous Vertebroplasty: The Embolus Broke in Half and Migrated to the Right Pulmonary Artery Intraoperatively
- Multidetector CT Findings of Polymethylmethacrylate Cement Leakage Inducing Inferior Vena Cava Thrombosis: A Case Report
- A Case of Fatal Pulmonary Embolism Caused by Bone Cement after Percutaneous Vertebroplasty