Clin Orthop Surg.
2010 Dec;2(4):256-259. 10.4055/cios.2010.2.4.256.
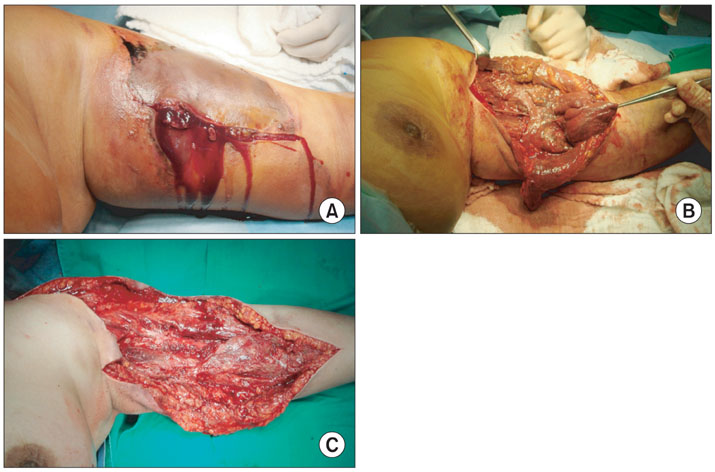
Coagulase-Positive Staphylococcal Necrotizing Fasciitis Subsequent to Shoulder Sprain in a Healthy Woman
- Affiliations
-
- 1Department of Orthopedic Surgery, Konkuk University School of Medicine, Chungju, Korea. kodukan@google.com
- KMID: 1719328
- DOI: http://doi.org/10.4055/cios.2010.2.4.256
Abstract
- Necrotizing fasciitis (NF) is a deep infection of the subcutaneous tissue that progressively destroys fascia and fat; it is associated with systemic toxicity, a fulminant course, and high mortality. NF most frequently develops from trauma that compromises skin integrity, and is more common in patients with predisposing medical conditions such as diabetes mellitus, atherosclerosis, alcoholism, renal disease, liver disease, immunosuppression, malignancy, or corticosteroid use. Most often, NF is caused by polymicrobial pathogens including aerobic and anaerobic bacteria. NF caused by Staphylococcus aureus as a single pathogen, however, is rare. Here we report a case of NF that developed in a healthy woman after an isolated shoulder sprain that occurred without breaking a skin barrier, and was caused by Staphylococcus aureus as a single pathogen.
Keyword
MeSH Terms
Figure
Reference
-
1. Brook I, Frazier EH. Clinical and microbiological features of necrotizing fasciitis. J Clin Microbiol. 1995. 33(9):2382–2387.
Article2. Fildes J, Bannon MP, Barrett J. Soft-tissue infections after trauma. Surg Clin North Am. 1991. 71(2):371–384.
Article3. Fisher JR, Conway MJ, Takeshita RT, Sandoval MR. Necrotizing fasciitis: importance of roentgenographic studies for soft-tissue gas. JAMA. 1979. 241(8):803–806.
Article4. Svensson LG, Brookstone AJ, Wellsted M. Necrotizing fasciitis in contused areas. J Trauma. 1985. 25(3):260–262.
Article5. Dunn F. Two cases of biceps injury in bodybuilders with initially misleading presentation. Emerg Med J. 2002. 19(5):461–462.
Article6. McHenry CR, Piotrowski JJ, Petrinic D, Malangoni MA. Determinants of mortality for necrotizing soft-tissue infections. Ann Surg. 1995. 221(5):558–563.
Article7. Wang KC, Shih CH. Necrotizing fasciitis of the extremities. J Trauma. 1992. 32(2):179–182.
Article