J Korean Med Sci.
2006 Dec;21(6):1054-1059. 10.3346/jkms.2006.21.6.1054.
Cost is a Barrier to Widespread Use of Liquid-Based Cytology for Cervical Cancer Screening in Korea
- Affiliations
-
- 1Department of Obstetrics and Gynecology, Seoul National University College of Medicine, 28 Yongon-dong, Chongno-gu, Seoul, Korea. kjwksh@snu.ac.kr
- KMID: 1713118
- DOI: http://doi.org/10.3346/jkms.2006.21.6.1054
Abstract
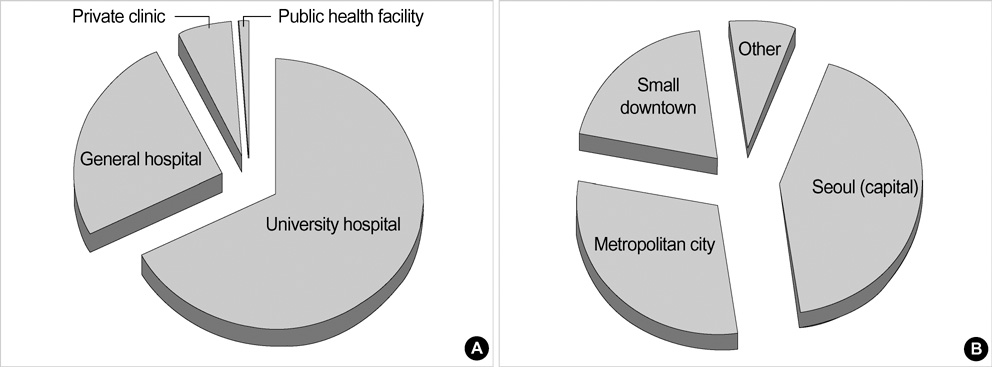
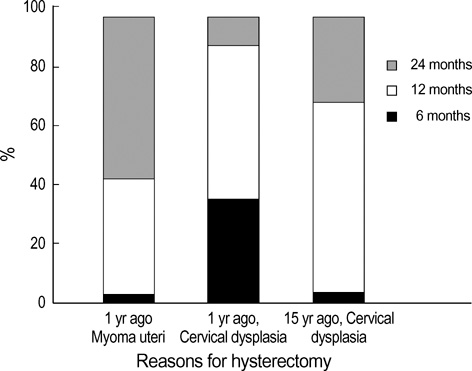
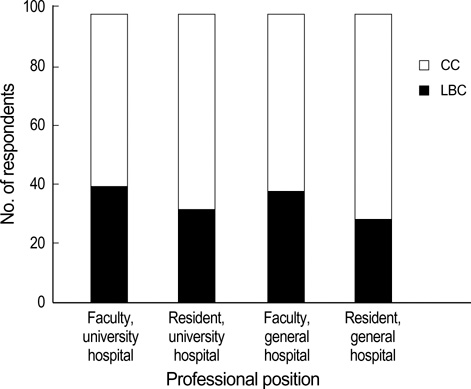
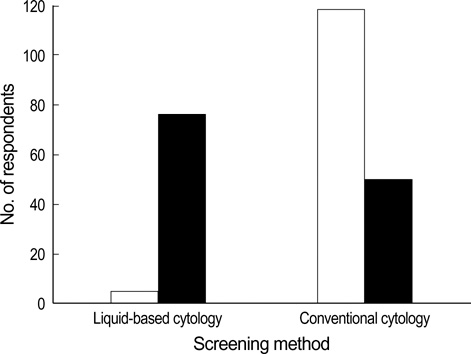
- This study aimed to document current cervical cancer screening practices of physicians in Korea. Questionnaires were distributed to 852 Korean obstetricians and gynecologists, who attended the 91st Conference of the Korean Society of Obstetrics and Gynecology held during May, 2005. Questionnaires were returned by 30.6% (260/852) of the recipients and 254 of these were eligible for analysis. Sixty-seven percent started cervical cancer screening women at age 20, and 65% replied that they would continue annual screening in a 35-yr-old woman with three consecutive normal cytologic tests. Over 65% of respondents preferred conventional cytologic screening to liquid-based cytology. The cost was a major determinant for selecting screening method. Fifty-three percent used the human papillomavirus DNA test as a triage for atypical squamous cells of undetermined significance. Our findings suggest that majority of Korean obstetricians and gynecologists in hospital prefer annual conventional cytologic testing to liquid-based cytology for financial reason.
Keyword
MeSH Terms
-
Uterine Cervical Neoplasms/*economics/epidemiology/*pathology
Questionnaires
Physician's Practice Patterns/*statistics & numerical data
Mass Screening/*economics/*statistics & numerical data
Male
Korea/epidemiology
Humans
Health Care Costs/statistics & numerical data
Female
Cytological Techniques/*statistics & numerical data
*Attitude of Health Personnel
Adult
Figure
Reference
-
1. Parkin DM, Bray F, Ferlay J, Pisani P. Estimating the world cancer burden: Globocan 2000. Int J Cancer. 2001. 94:153–156.
Article2. Ministry of Health and Welfare. 2002 Annual report of Korea Central Cancer Registry. 2003. Seoul:3. Devesa SS, Young JL Jr, Brinton LA, Fraumeni JF Jr. Recent trends in cervix uteri cancer. Cancer. 1989. 64:2184–2190.
Article4. Eide TJ. Cancer of the uterine cervix in Norway by histologic type, 1970-84. J Natl Cancer Inst. 1987. 79:199–205.5. Nieminen P, Kallio M, Hakama M. The effect of mass screening on incidence and mortality of squamous and adenocarcinoma of cervix uteri. Obstet Gynecol. 1995. 85:1017–1021.
Article6. Coleman MP, Esteve J, Damiecki P, Arslan A, Renard H. Trends in cancer incidence and mortality. IARC Sci Publ. 1993. (121):1–806.7. Beral V, Hermon C, Munoz N, Devesa SS. Cervical cancer. Cancer Surv. 1994. 19-20:265–285.8. Benedet JL, Odicino F, Maisonneuve P, Beller U, Creasman WT, Heintz AP, Ngan HY, Pecorelli S. Carcinoma of the cervix uteri. Int J Gynaecol Obstet. 2003. 83:Suppl 1. 41–78.
Article9. Cannistra SA, Niloff JM. Cancer of the uterine cervix. N Engl J Med. 1996. 334:1030–1038.
Article10. Saslow D, Runowicz CD, Solomon D, Moscicki AB, Smith RA, Eyre HJ, Cohen C. American Cancer Society guideline for the early detection of cervical neoplasia and cancer. CA Cancer J Clin. 2002. 52:342–362.
Article11. ACOG Committee on Practice Bulletin: clinical management guidelines for obstetrician-gynecologists. Number 45, August 2003. Cervical cytology screening (replaces committee opinion 152, March 1995). Obstet Gynecol. 2003. 102:417–427.12. Sirovich BE, Woloshin S, Schwartz LM. Screening for cervical cancer: will women accept less? Am J Med. 2005. 118:151–158.
Article13. Sawaya GF, McConnell KJ, Kulasingam SL, Lawson HW, Kerlikowske K, Melnikow J, Lee NC, Gildengorin G, Myers ER, Washington AE. Risk of cervical cancer associated with extending the interval between cervical-cancer screenings. N Engl J Med. 2003. 349:1501–1509.
Article14. Longatto Filho A, Pereira SM, Di Loreto C, Utagawa ML, Makabe S, Sakamoto Maeda MY, Marques JA, Santoro CL, Castelo A. DCS liquid-based system is more effective than conventional smears to diagnosis of cervical lesions: study in high-risk population with biopsy-based confirmation. Gynecol Oncol. 2005. 97:497–500.15. Abulafia O, Pezzullo JC, Sherer DM. Performance of ThinPrep liquid-based cervical cytology in comparison with conventionally prepared Papanicolaou smears: a quantitative survey. Gynecol Oncol. 2003. 90:137–144.
Article16. Lim YK, Lim JC, Kim JH, Lee JP, Chang KH, Ju HJ, Ryu HS. Comparison of efficacy between MonoPrep(R) and Papanicolaou smear for cervical cancer screening. Korean J Obstet Gynecol. 2004. 47:109–117.17. Lee KC, Choi HS, Kim HJ, Kim YS, Jeong KP, Park H, Rim SY, Kim SM, Byun JS, Nam JH, Park CS. The comparison of conventional Pap smear with ThinPrep Pap smear in detecting HSIL and cervix cancer. Korean J Obstet Gynecol. 2002. 45:753–758.18. Noller KL, Bettes B, Zinberg S, Schulkin J. Cervical cytology screening practices among obstetrician-gynecologists. Obstet Gynecol. 2003. 102:259–265.
Article19. Saint M, Gildengorin G, Sawaya GF. Current cervical neoplasia screening practices of obstetrician/gynecologists in the US. Am J Obstet Gynecol. 2005. 192:414–421.
Article20. Harkness CB, Theofrastous JP, Ibrahim SN, Galvin SL, Lawrence HC. Papanicolaou and thin-layer cervical cytology with colposcopic biopsy control. A comparison. J Reprod Med. 2003. 48:681–686.21. Taylor S, Kuhn L, Dupree W, Denny L, De Souza M, Wright TC Jr. Direct comparison of liquid-based and conventional cytology in a South African screening trial. Int J Cancer. 2006. 118:957–962.
Article22. Sirovich BE, Welch HG. Cervical cancer screening among women without a cervix. JAMA. 2004. 291:2990–2993.
Article23. Group A-LTSA. Results of a randomized trial on the management of cytology interpretations of atypical squamous cells of undetermined significance. Am J Obstet Gynecol. 2003. 188:1383–1392.24. Kim JJ, Wright TC, Goldie SJ. Cost-effectiveness of alternative triage strategies for atypical squamous cells of undetermined significance. JAMA. 2002. 287:2382–2390.
Article25. Solomon D, Schiffman M, Tarone R. Comparison of three management strategies for patients with atypical squamous cells of undetermined significance: baseline results from a randomized trial. J Natl Cancer Inst. 2001. 93:293–299.
Article26. Stoler MH, Schiffman M. Interobserver reproducibility of cervical cytologic and histologic interpretations: realistic estimates from the ASCUS-LSIL Triage Study. JAMA. 2001. 285:1500–1505.27. Sherman ME, Lorincz AT, Scott DR, Wacholder S, Castle PE, Glass AG, Mielzynska-Lohnas I, Rush BB, Schiffman M. Baseline cytology, human papillomavirus testing, and risk for cervical neoplasia: a 10-year cohort analysis. J Natl Cancer Inst. 2003. 95:46–52.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Liquid-Based Cytology in Gynecologic Cytology
- The efficacy of a real-time optoelectronic device as a diagnostic tool of over cervical intraepithelial neoplasia 1 lesion
- The Clinical Evaluation of Triple Combined Test [ Cytology, HPV DNA Test, Cervicography] for Uterine Cervical Cancer
- Diagnostic accuracy of conventional Pap test, liquid-based cytology and human papillomavirus DNA testing in cervical cancer screening in Korea: a meta-analysis
- The Usefulness of Cervicovaginal Cytology as a Primary Screening Test