J Cardiovasc Ultrasound.
2013 Sep;21(3):130-136. 10.4250/jcu.2013.21.3.130.
Acute Effect of Whole-Body Periodic Acceleration on Brachial Flow-Mediated Vasodilatation Assessed by a Novel Semi-Automatic Vessel Chasing UNEXEF18G System
- Affiliations
-
- 1Department of Intensive Care Medicine, National Defense Medical College, National Defense Medical College Research Institute, Saitama, Japan. bonpeit@ndmc.ac.jp
- 2Division of Biomedical Engineering, National Defense Medical College, National Defense Medical College Research Institute, Saitama, Japan.
- 3Self Defense Forces Central Hospital, Tokyo, Japan.
- 4Iruma Heart Hospital, Saitama, Japan.
- 5Human Health Sciences, Kyoto University Graduate School of Medicine, Kyoto, Japan.
- KMID: 1500192
- DOI: http://doi.org/10.4250/jcu.2013.21.3.130
Abstract
- BACKGROUND
Repeated application of whole-body periodic acceleration (WBPA) upregulates endothelial nitric oxide synthase and improves brachial artery endothelial function (BAEF) as assessed by measurement of flow-mediated vasodilatation (FMD). However, the acute effect of a single application of WBPA on BAEF has not been fully characterized. In addition, although a novel semi-automatic vessel chasing system (UNEXEF18G) has now been developed in Japan, the direct comparison of UNEXEF18G with a conventional method for FMD measures has not been conducted even if UNEXEF18G has already been utilized in a relatively large scale study.
METHODS
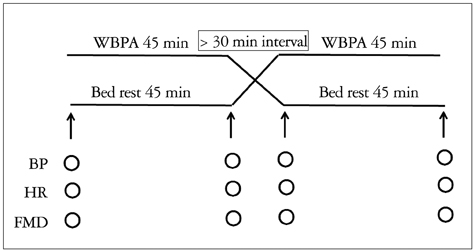
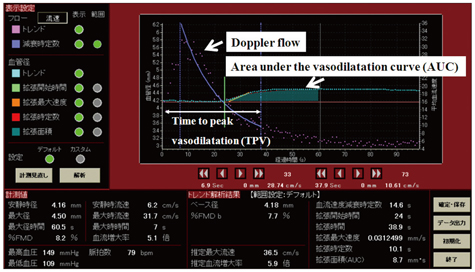
We have developed a novel semi-automatic vessel chasing system (UNEXEF18G) that can measure FMD on-line, identify time to peak vasodilatation (TPV), and determine the area under the vasodilatation curve (AUC). Thus, 45 min of WBPA was applied in 20 healthy volunteers (age, 34 +/- 13 years), and BAEF was measured by UNEXEF18G before and after WBPA. Also, UNEXEF18G measured FMD was compared with those of a conventional FMD measurement method at rest in order to validate a novel UNEXEF18G measured FMD.
RESULTS
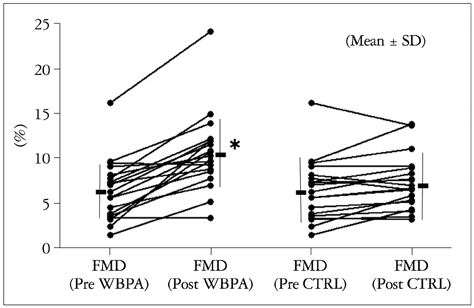
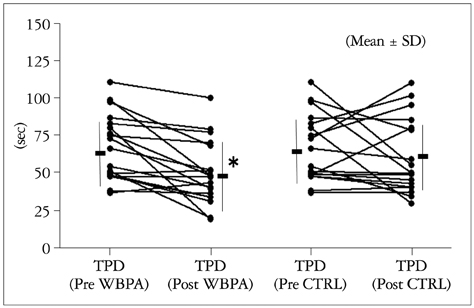
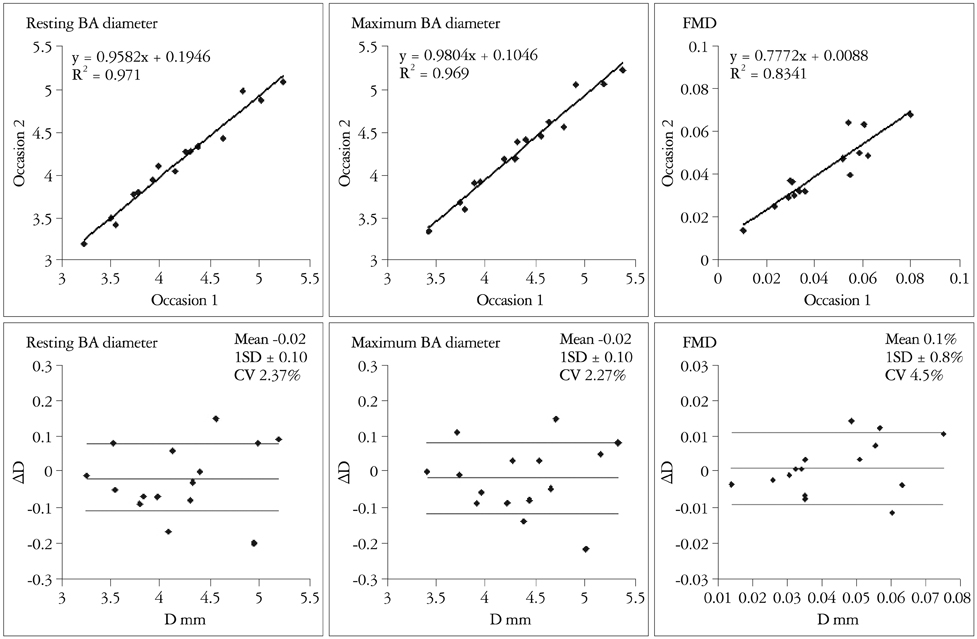
Single WBPA resulted in a significant increase in FMD (from 6.4 +/- 3.4 to 10.7 +/- 4.3%, p < 0.01), a significant decrease in TPV and a significant increase in AUC. In the validation study for UNEXEF18G, Bland and Altman analysis showed that UNEXEF18G measured FMD was almost identical to those of the conventional method at rest.
CONCLUSION
These data suggest the usefulness of a new UNEXEF18G and that single application of WBPA results in acute improvement in BAEF in humans.
MeSH Terms
Figure
Reference
-
1. Philpott AC, Lonn E, Title LM, Verma S, Buithieu J, Charbonneau F, Anderson TJ. Comparison of new measures of vascular function to flow mediated dilatation as a measure of cardiovascular risk factors. Am J Cardiol. 2009; 103:1610–1615.
Article2. Reriani MK, Lerman LO, Lerman A. Endothelial function as a functional expression of cardiovascular risk factors. Biomark Med. 2010; 4:351–360.
Article3. Hambrecht R, Adams V, Erbs S, Linke A, Kränkel N, Shu Y, Baither Y, Gielen S, Thiele H, Gummert JF, Mohr FW, Schuler G. Regular physical activity improves endothelial function in patients with coronary artery disease by increasing phosphorylation of endothelial nitric oxide synthase. Circulation. 2003; 107:3152–3158.
Article4. Kang JL, Park W, Pack IS, Lee HS, Kim MJ, Lim CM, Koh Y. Inhaled nitric oxide attenuates acute lung injury via inhibition of nuclear factor-kappa B and inflammation. J Appl Physiol. 2002; 92:795–801.
Article5. Pipili-Synetos E, Papageorgiou A, Sakkoula E, Sotiropoulou G, Fotsis T, Karakiulakis G, Maragoudakis ME. Inhibition of angiogenesis, tumour growth and metastasis by the NO-releasing vasodilators, isosorbide mononitrate and dinitrate. Br J Pharmacol. 1995; 116:1829–1834.
Article6. Sackner MA, Gummels E, Adams JA. Nitric oxide is released into circulation with whole-body, periodic acceleration. Chest. 2005; 127:30–39.
Article7. Fukuda S, Shimada K, Kawasaki T, Kono Y, Jissho S, Taguchi H, Maeda K, Yoshiyama M, Fujita M, Yoshikawa J. "Passive exercise" using whole body periodic acceleration: effects on coronary microcirculation. Am Heart J. 2010; 159:620–626.
Article8. Tomiyama H, Matsumoto C, Yamada J, Teramoto T, Abe K, Ohta H, Kiso Y, Kawauchi T, Yamashina A. The relationships of cardiovascular disease risk factors to flow-mediated dilatation in Japanese subjects free of cardiovascular disease. Hypertens Res. 2008; 31:2019–2025.
Article9. Tomiyama H, Kohro T, Higashi Y, Takase B, Suzuki T, Ishizu T, Ueda S, Yamazaki T, Furumoto T, Kario K, Inoue T, Koba S, Watanabe K, Takemoto Y, Hano T, Sata M, Ishibashi Y, Node K, Maemura K, Ohya Y, Furukawa T, Ito H, Yamashina A. A multicenter study design to assess the clinical usefulness of semi-automatic measurement of flow-mediated vasodilatation of the brachial artery. Int Heart J. 2012; 53:170–175.
Article10. Hamabe A, Takase B, Uehata A, Kurita A, Ohsuzu F, Tamai S. Impaired endothelium-dependent vasodilation in the brachial artery in variant angina pectoris and the effect of intravenous administration of vitamin C. Am J Cardiol. 2001; 87:1154–1159.
Article11. Takase B, Akima T, Uehata A, Ohsuzu F, Kurita A. Effect of chronic stress and sleep deprivation on both flow-mediated dilation in the brachial artery and the intracellular magnesium level in humans. Clin Cardiol. 2004; 27:223–227.
Article12. Bland JM, Altman DG. Statistical methods for assessing agreement between two methods of clinical measurement. Lancet. 1986; 1:307–310.
Article13. Bland JM, Altman DG. Agreed statistics: measurement method comparison. Anesthesiology. 2012; 116:182–185.14. Padilla J, Johnson BD, Newcomer SC, Wilhite DP, Mickleborough TD, Fly AD, Mather KJ, Wallace JP. Normalization of flow-mediated dilation to shear stress area under the curve eliminates the impact of variable hyperemic stimulus. Cardiovasc Ultrasound. 2008; 6:44.
Article15. Peretz A, Leotta DF, Sullivan JH, Trenga CA, Sands FN, Aulet MR, Paun M, Gill EA, Kaufman JD. Flow mediated dilation of the brachial artery: an investigation of methods requiring further standardization. BMC Cardiovasc Disord. 2007; 7:11.
Article16. Black MA, Cable NT, Thijssen DH, Green DJ. Importance of measuring the time course of flow-mediated dilatation in humans. Hypertension. 2008; 51:203–210.
Article17. Celermajer DS, Sorensen K, Ryalls M, Robinson J, Thomas O, Leonard JV, Deanfield JE. Impaired endothelial function occurs in the systemic arteries of children with homozygous homocystinuria but not in their heterozygous parents. J Am Coll Cardiol. 1993; 22:854–858.
Article18. Thijssen DH, Black MA, Pyke KE, Padilla J, Atkinson G, Harris RA, Parker B, Widlansky ME, Tschakovsky ME, Green DJ. Assessment of flow-mediated dilation in humans: a methodological and physiological guideline. Am J Physiol Heart Circ Physiol. 2011; 300:H2–H12.
Article19. Uehata A, Lieberman EH, Gerhard MD, Anderson TJ, Ganz P, Polak JF, Creager MA, Yeung AC. Noninvasive assessment of endothelium-dependent flow-mediated dilation of the brachial artery. Vasc Med. 1997; 2:87–92.
Article20. Anderson TJ, Uehata A, Gerhard MD, Meredith IT, Knab S, Delagrange D, Lieberman EH, Ganz P, Creager MA, Yeung AC, et al. Close relation of endothelial function in the human coronary and peripheral circulations. J Am Coll Cardiol. 1995; 26:1235–1241.
Article21. Green DJ, Jones H, Thijssen D, Cable NT, Atkinson G. Flow-mediated dilation and cardiovascular event prediction: does nitric oxide matter? Hypertension. 2011; 57:363–369.
Article22. Sessa WC. Regulation of endothelial derived nitric oxide in health and disease. Mem Inst Oswaldo Cruz. 2005; 100:Suppl 1. 15–18.
Article23. Förstermann U, Münzel T. Endothelial nitric oxide synthase in vascular disease: from marvel to menace. Circulation. 2006; 113:1708–1714.24. Jones SP, Bolli R. The ubiquitous role of nitric oxide in cardioprotection. J Mol Cell Cardiol. 2006; 40:16–23.
Article25. Belge C, Massion PB, Pelat M, Balligand JL. Nitric oxide and the heart: update on new paradigms. Ann N Y Acad Sci. 2005; 1047:173–182.
Article26. Nathan C. Points of control in inflammation. Nature. 2002; 420:846–852.
Article27. Takase B, Nagata M, Hujita M. Acute effect of whole-body periodic acceleration on cardiac autonomic function and brachial endothelial function. J Arrhythm. 2012; 28:Supplement. 546.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Mitral Doppler Flow, Flow Propagation Velocity and Peak Filling Rate between Patients with Normal and Systolic LV Dysfunction in Presence of Atrial Fibrillation
- Modelling of Elastic Blood Vessel under the Pulsatile Flow
- Endothelial Function is Not Changed during Short-Term Withdrawal of Thyroxine in Patients with Differentiated Thyroid Cancer and Low Cardiovascular Risk
- The Effect of Norepinephrine on Blood Pressure and Blood Flow of the Brachial and Femoral Arteries
- The Effect of Acute Aerobic Exercise on Central Blood Pressure Reactivity to Sympathetic Activation in Healthy Adults: A Randomized Crossover Trial