J Korean Fract Soc.
2013 Apr;26(2):164-169. 10.12671/jkfs.2013.26.2.164.
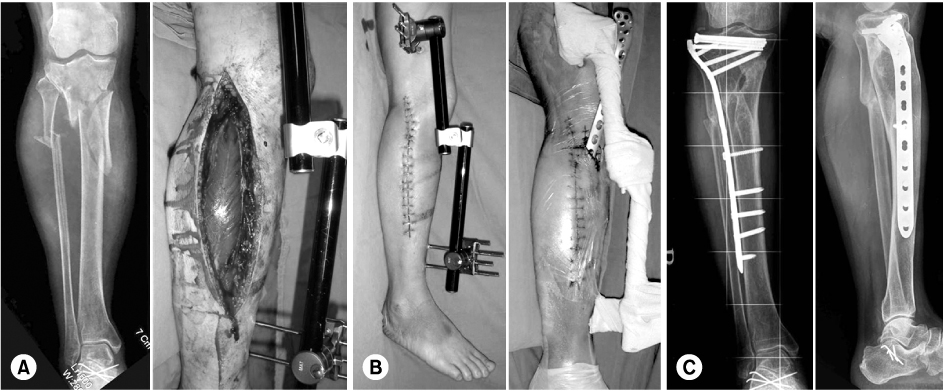
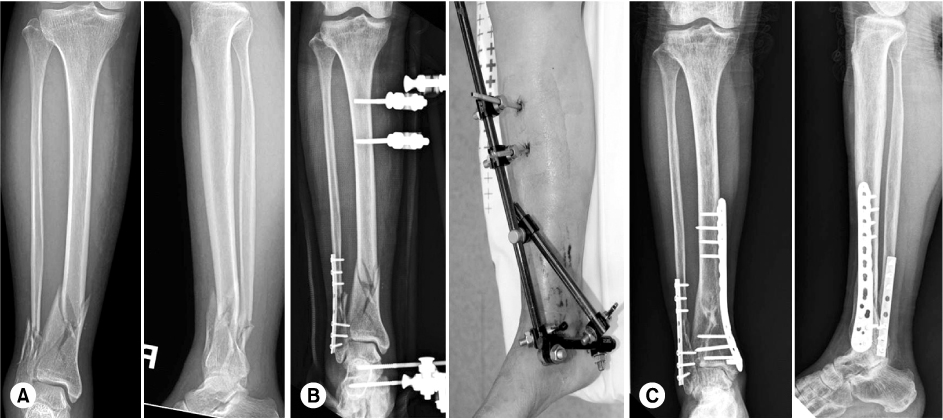
Selection and Recommended Usage Guide of Temporary External Fixator
- Affiliations
-
- 1Department of Orthopedic Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. limsj@skku.edu
- 2Department of Orthopedic Surgery, Kyungpook National University Hospital, Kyungpook National University Medical School, Daegu, Korea.
- KMID: 1496173
- DOI: http://doi.org/10.12671/jkfs.2013.26.2.164
Abstract
- No abstract available.
MeSH Terms
Figure
Reference
-
1. Anglen JO. Early outcome of hybrid external fixation for fracture of the distal tibia. J Orthop Trauma. 1999. 13:92–97.
Article2. Anglen JO, Aleto T. Temporary transarticular external fixation of the knee and ankle. J Orthop Trauma. 1998. 12:431–434.
Article3. Barei DP, Nork SE, Mills WJ, Henley MB, Benirschke SK. Complications associated with internal fixation of high-energy bicondylar tibial plateau fractures utilizing a two-incision technique. J Orthop Trauma. 2004. 18:649–657.
Article4. Behrens F. General theory and principles of external fixation. Clin Orthop Relat Res. 1989. (241):15–23.
Article5. Blauth M, Bastian L, Krettek C, Knop C, Evans S. Surgical options for the treatment of severe tibial pilon fractures: a study of three techniques. J Orthop Trauma. 2001. 15:153–160.
Article6. Casey D, McConnell T, Parekh S, Tornetta P 3rd. Percutaneous pin placement in the medial calcaneus: is anywhere safe? J Orthop Trauma. 2002. 16:26–29.
Article7. Chen SH, Wu PH, Lee YS. Long-term results of pilon fractures. Arch Orthop Trauma Surg. 2007. 127:55–60.
Article8. Collinge C, Kennedy J, Schmidt A. Temporizing external fixation of the lower extremity: a survey of the Orthopaedic Trauma Association Membership. Orthopedics. 2010. 239–244. [Epub ahead of print].
Article9. Dillin L, Slabaugh P. Delayed wound healing, infection, and nonunion following open reduction and internal fixation of tibial plafond fractures. J Trauma. 1986. 26:1116–1119.
Article10. Haidukewych GJ. Temporary external fixation for the management of complex intra- and periarticular fractures of the lower extremity. J Orthop Trauma. 2002. 16:678–685.
Article11. Lau TW, Leung F, Chan CF, Chow SP. Wound complication of minimally invasive plate osteosynthesis in distal tibia fractures. Int Orthop. 2008. 32:697–703.
Article12. Oh CW, Lee HJ. Acute compartment syndrome after trauma. J Korean Fract Soc. 2010. 23:399–403.
Article13. Oh JK, Hwang JH, Sahu D, Jun SH. Complication rate and pitfalls of temporary bridging external fixator in periarticular communited fractures. Clin Orthop Surg. 2011. 3:62–68.
Article14. Patterson MJ, Cole JD. Two-staged delayed open reduction and internal fixation of severe pilon fractures. J Orthop Trauma. 1999. 13:85–91.
Article15. Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma. 2007. 21:83–91.
Article16. Sirkin M, Sanders R, DiPasquale T, Herscovici D Jr. A staged protocol for soft tissue management in the treatment of complex pilon fractures. J Orthop Trauma. 2004. 18:S32–S38.
Article17. Sohn OJ, Kang DH. Staged protocol in treatment of open distal tibia fracture: using lateral MIPO. Clin Orthop Surg. 2011. 3:69–76.
Article18. Watson JT, Moed BR, Karges DE, Cramer KE. Pilon fractures. Treatment protocol based on severity of soft tissue injury. Clin Orthop Relat Res. 2000. (375):78–90.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Staged Treatment of Bicondylar Tibial Plateau Fracture (Schatzker Type V or VI) Using Temporary External Fixator: Correlation between Clinical and Radiological Outcomes
- Cross-Leg Flap Imobilized with External Fixator Brace
- Rupture of Femoral Artery by External Fixator
- A Clinical Analysis on Treatment of Tibial Fractures Using Ex-Fi-Re External Fixator
- Treatment of Wrist Frarture-Disluation using the Mini-External Fixator and Internal Fixation