J Korean Orthop Assoc.
2013 Oct;48(5):375-381. 10.4055/jkoa.2013.48.5.375.
Comparison of Clinical Results according to the Complications after or during Open Door Laminoplasty Surgery for Cervical Myelopathy
- Affiliations
-
- 1Department of Orthopedic Surgery, Chungnam National University School of Medicine, Daejeon, Korea. jsahn@cnu.ac.kr
- KMID: 1494150
- DOI: http://doi.org/10.4055/jkoa.2013.48.5.375
Abstract
- PURPOSE
The purpose of this study is to compare and analyze the clinical results according to the complications occurring after laminoplasty for cervical myelopathy patients.
MATERIALS AND METHODS
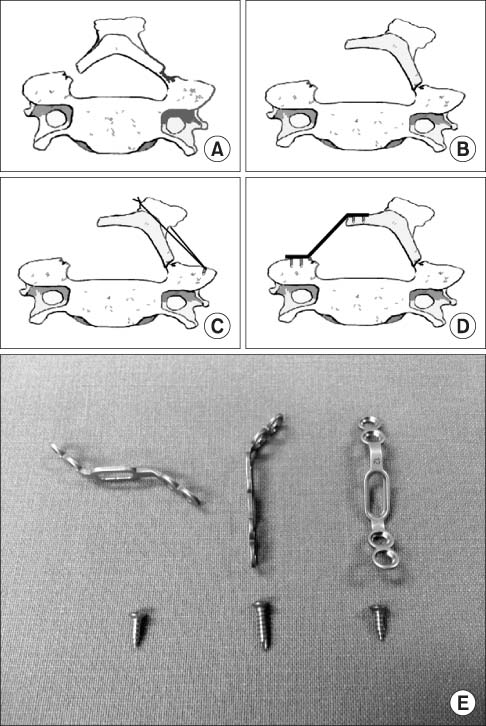
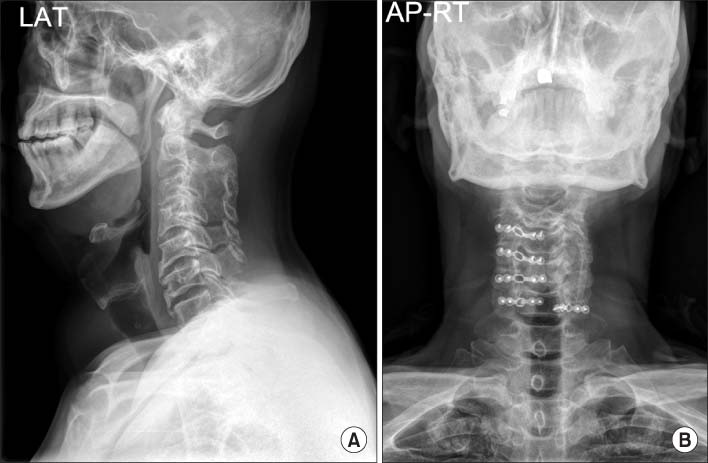
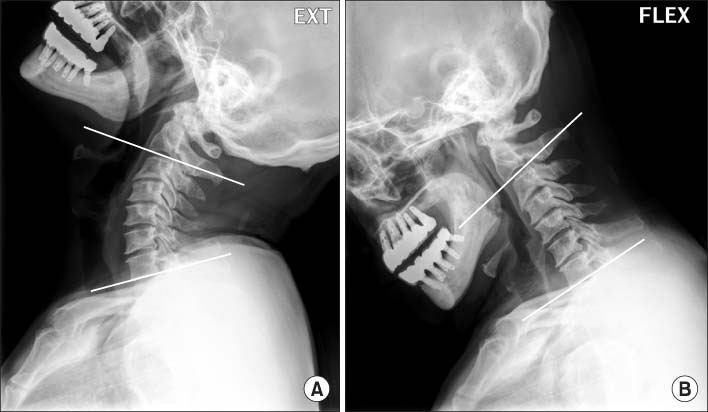
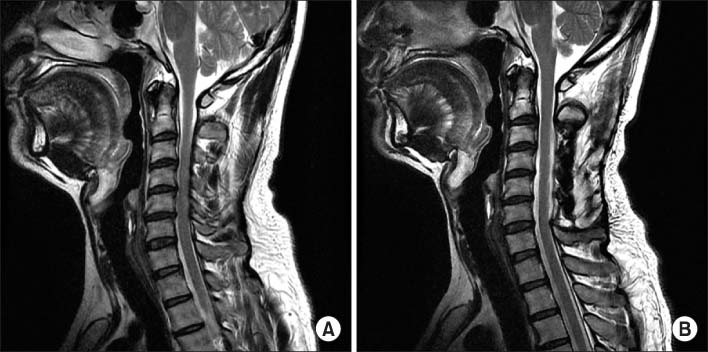
Among patients diagnosed as cervical myelopathy, 152 cases in which patients underwent cervical laminoplasty from March 2006 to March 2011 from Chungnam National University Hospital and had follow-up for at least two years were selected for the study, and the mean follow-up period was 39.7 months. The cases were divided into two groups; cases that underwent plate fixation for hinge fracture during cervical laminoplasty or showed postoperative spontaneous interlamina fusion were included in group A and cases that did not show such complications were included in group B. Clinical results were measured using visual analogue scale (VAS) score and Neck Disability Index (NDI) preoperatively, postoperatively, and on the final follow-up.
RESULTS
Among 152 cases, 31 cases were included in group A and 121 cases in group B. Group A consisted of 11 cases of fixation due to intraoperative hinge fracture and 20 cases of postoperative spontaneous interlamina fusion. Mean preoperative VAS score was 7.52 in group A and 7.26 in group B, and mean postoperative VAS score was 2.87 in group A and 3.03 in group B. Mean NDI improved from 74.32% preoperatively to 43.84% postoperatively in group A and 75.74% preoperatively to 45.36% postoperatively in group B. In both groups, on postoperative follow-up, no significant difference of VAS score and NDI was found and both showed improvement compared to before surgery.
CONCLUSION
The clinical results of cases that underwent plate fixation for hinge fracture that occurred during cervical laminoplasty and postoperative spontaneous interlamina fusion showed no significant difference compared to cases that did not show any complications.
Figure
Reference
-
1. Chang H. Cervical spondylotic myelopathy. J Korean Soc Spine Surg. 1999; 6:194–200.2. Hosono N, Yonenobu K, Ono K. Neck and shoulder pain after laminoplasty. A noticeable complication. Spine (Phila Pa 1976). 1996; 21:1969–1973.3. Kawaguchi Y, Kanamori M, Ishihara H, et al. Progression of ossification of the posterior longitudinal ligament following en bloc cervical laminoplasty. J Bone Joint Surg Am. 2001; 83:1798–1802.
Article4. Edwards CC 2nd, Heller JG, Silcox DH 3rd. T-saw laminoplasty for the management of cervical spondylotic myelopathy: clinical and radiographic outcome. Spine (Phila Pa 1976). 2000; 25:1788–1794.5. Satomi K, Nishu Y, Kohno T, Hirabayashi K. Long-term follow-up studies of open-door expansive laminoplasty for cervical stenotic myelopathy. Spine (Phila Pa 1976). 1994; 19:507–510.
Article6. Wada E, Suzuki S, Kanazawa A, Matsuoka T, Miyamoto S, Yonenobu K. Subtotal corpectomy versus laminoplasty for multilevel cervical spondylotic myelopathy: a long-term follow-up study over 10 years. Spine (Phila Pa 1976). 2001; 26:1443–1447.7. Zdeblick TA, Abitbol JJ, Kunz DN, McCabe RP, Garfin S. Cervical stability after sequential capsule resection. Spine (Phila Pa 1976). 1993; 18:2005–2008.
Article8. Zdeblick TA, Zou D, Warden KE, McCabe R, Kunz D, Vanderby R. Cervical stability after foraminotomy. A biomechanical in vitro analysis. J Bone Joint Surg Am. 1992; 74:22–27.
Article9. Shaffrey CI, Wiggins GC, Piccirilli CB, Young JN, Lovell LR. Modified open-door laminoplasty for treatment of neurological deficits in younger patients with congenital spinal stenosis: analysis of clinical and radiographic data. J Neurosurg. 1999; 90:170–177.
Article10. Hirabayashi K, Bohlman HH. Multilevel cervical spondylosis. Laminoplasty versus anterior decompression. Spine (Phila Pa 1976). 1995; 20:1732–1734.11. Ahn JS, Lee JK, Lee WW, Hwang JM. Changes in cervical spine range of motion after laminoplasty in cervical spondylotic myelopathy. J Korean Soc Spine Surg. 2012; 19:85–89.
Article12. Suk KS, Kim KT, Lee SH, Lim YJ, Lee KW. Changes of range of motion and sagittal alignment of the cervical spine after laminoplasty. J Korean Soc Spine Surg. 2005; 12:247–254.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Early Surgical Outcome between Unilateral Open-Door Laminoplasty and Midline Splitting Laminoplasty
- Original Surgical Treatment and Long-term Follow-up for Chronic Inflammatory Demyelinating Polyradiculoneuropathy Causing a Compressive Cervical Myelopathy: Review of the Literature
- Technical Modification and Comparison of Results with Hirabayashi's Open-door Laminoplasty
- Comparison of Midline Splitting versus Unilateral Open Door Laminoplasty and Its Impact on Patient Outcomes
- Cervical Laminoplasty Using Titanium Miniplate