J Korean Orthop Assoc.
2013 Oct;48(5):366-374. 10.4055/jkoa.2013.48.5.366.
Comparison of Clinical Results and Second-Look Arthroscopic Findings of Remnant Preserving versus Non-Remnant Preserving Technique after Anterior Cruciate Ligament Reconstruction Using Achilles Allograft
- Affiliations
-
- 1Department of Orthopedic Surgery, Wonkwang University School of Medicine, Iksan, Korea. cch@wonkwang.ac.kr
- 2Department of Nursing, Chodang University, Muan, Korea.
- KMID: 1494149
- DOI: http://doi.org/10.4055/jkoa.2013.48.5.366
Abstract
- PURPOSE
This study was conducted for evaluation of clinical uses of anterior cruciate ligament (ACL) reconstruction with an Achilles allograft using the remnant technique by comparison and analysis stability, functional assessment and results of second-look arthroscopy between the remnant technique and the non-remnanat technique.
MATERIALS AND METHODS
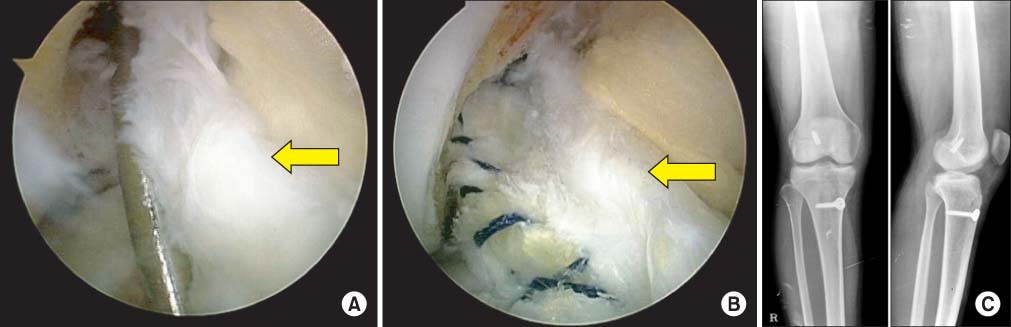
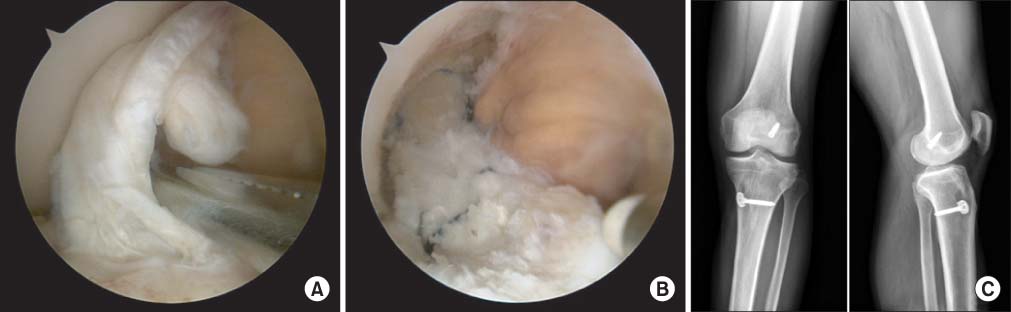
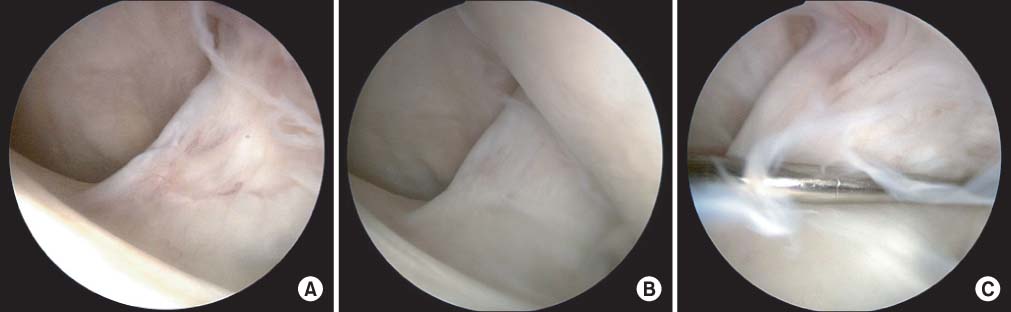
A total of 48 patients who underwent ACL reconstruction using an Achilles allograft were selected and divided into two groups depending on the presence of remnant. The preserving group included 26 patients and non-preserving group included 22 patients. The two groups were compared and analyzed with regarding to stability (Stress view Lachman test, pivot shift test), functional assessment (International Knee Documentation Committee, Lysholm score, Tegner score, single hoop test, shuttle turn, carioca test), and the result of second-look arthroscopy (study design: prosepective cohort study).
RESULTS
In the final result, the remnant group showed significant improvement in the Tegner and carioca tests compared with the non-remnant group (p<0.05). In second-look arthroscopy, the remnant group showed better coverage of synovium (p<0.05).
CONCLUSION
ACL reconstruction with an Achilles allograft using the remnant technique showed better results in functional assessment and finding in second-look arthroscopy compared with the non-remnant technique group.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Comparison of Magnetic Resonance Imaging of Remnant Preserving versus Remnant Sacrificing Technique after Anterior Cruciate Ligament Reconstruction; Clinical Results and Second-Look Arthroscopic Findings: Pilot Study
Byung-Ill Lee, Byoung-Min Kim, Duk-Hwan Kho, Sai-Won Kwon, Hwan-Bae Kim
J Korean Orthop Assoc. 2015;50(6):501-512. doi: 10.4055/jkoa.2015.50.6.501.
Reference
-
1. Lewis PB, Parameswaran AD, Rue JP, Bach BR Jr. Systematic review of single-bundle anterior cruciate ligament reconstruction outcomes: a baseline assessment for consideration of double-bundle techniques. Am J Sports Med. 2008; 36:2028–2036.2. Barrett DS. Proprioception and function after anterior cruciate reconstruction. J Bone Joint Surg Br. 1991; 73:833–837.
Article3. Fremerey RW, Lobenhoffer P, Zeichen J, Skutek M, Bosch U, Tscherne H. Proprioception after rehabilitation and reconstruction in knees with deficiency of the anterior cruciate ligament: a prospective, longitudinal study. J Bone Joint Surg Br. 2000; 82:801–806.4. Reider B, Arcand MA, Diehl LH, et al. Proprioception of the knee before and after anterior cruciate ligament reconstruction. Arthroscopy. 2003; 19:2–12.
Article5. Shimizu T, Takahashi T, Wada Y, Tanaka M, Morisawa Y, Yamamoto H. Regeneration process of mechanoreceptors in the reconstructed anterior cruciate ligament. Arch Orthop Trauma Surg. 1999; 119:405–409.
Article6. Barrack RL, Skinner HB, Buckley SL. Proprioception in the anterior cruciate deficient knee. Am J Sports Med. 1989; 17:1–6.
Article7. Lee BI, Min KD, Yoon ES, Kim JB, Choi HS, Lee DH. Mechanoreceptors in the remnants of ruptured anterior cruciate ligaments in human knees. J Korean Orthop Assoc. 2006; 41:811–817.
Article8. Shelbourne KD, Nitz P. Accelerated rehabilitation after anterior cruciate ligament reconstruction. J Orthop Sports Phys Ther. 1992; 15:256–264.
Article9. Anderson AF, Rennirt GW, Standeffer WC Jr. Clinical analysis of the pivot shift tests: description of the pivot drawer test. Am J Knee Surg. 2000; 13:19–23.10. Chun CH, Lee BC, Yang JH. Extension block secondary to partial anterior cruciate ligament tear on the femoral attachment of the posterolateral bundle. Arthroscopy. 2002; 18:227–231.
Article11. Jackson DW, Windler GE, Simon TM. Intraarticular reaction associated with the use of freeze-dried, ethylene oxide-sterilized bone-patella tendon-bone allografts in the reconstruction of the anterior cruciate ligament. Am J Sports Med. 1990; 18:1–10.
Article12. Roberts TS, Drez D Jr, McCarthy W, Paine R. Anterior cruciate ligament reconstruction using freeze-dried, ethylene oxide-sterilized, bone-patellar tendon-bone allografts. Two year results in thirty-six patients. Am J Sports Med. 1991; 19:35–41.13. Peterson RK, Shelton WR, Bomboy AL. Allograft versus autograft patellar tendon anterior cruciate ligament reconstruction: a 5-year follow-up. Arthroscopy. 2001; 17:9–13.14. Linn RM, Fischer DA, Smith JP, Burstein DB, Quick DC. Achilles tendon allograft reconstruction of the anterior cruciate ligament-deficient knee. Am J Sports Med. 1993; 21:825–831.
Article15. Schultz RA, Miller DC, Kerr CS, Micheli L. Mechanoreceptors in human cruciate ligaments. A histological study. J Bone Joint Surg Am. 1984; 66:1072–1076.
Article16. Beard DJ, Kyberd PJ, Fergusson CM, Dodd CA. Proprioception after rupture of the anterior cruciate ligament. An objective indication of the need for surgery? J Bone Joint Surg Br. 1993; 75:311–315.
Article17. Corrigan JP, Cashman WF, Brady MP. Proprioception in the cruciate deficient knee. J Bone Joint Surg Br. 1992; 74:247–250.
Article18. Kim SH, Chun CH, Chun KC, Jo HJ, Kim KM. Histological assessment of mechanoreceptors in Achilles allografts after anterior cruciate ligament reconstruction. Am J Sports Med. 2012; 40:2061–2065.
Article19. Chun CH, Han HJ, Lee BC, Kim DC, Yang JH. Histologic findings of anterior cruciate ligament reconstruction with Achilles allograft. Clin Orthop Relat Res. 2004; 421:273–276.
Article20. Ochi M, Adachi N, Deie M, Kanaya A. Anterior cruciate ligament augmentation procedure with a 1-incision technique: anteromedial bundle or posterolateral bundle reconstruction. Arthroscopy. 2006; 22:463.
Article21. Crain EH, Fithian DC, Paxton EW, Luetzow WF. Variation in anterior cruciate ligament scar pattern: does the scar pattern affect anterior laxity in anterior cruciate ligament-deficient knees? Arthroscopy. 2005; 21:19–24.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Proprioceptive and Knee Joint Kinematics for Comparison of Remnant Preserved versus Non-remnant Anterior Cruciate Ligament Reconstruction Using Achilles Allograft
- A Comparative Study of Clinical Outcomes and Second-Look Arthroscopic Findings between Remnant-Preserving Tibialis Tendon Allograft and Hamstring Tendon Autograft in Anterior Cruciate Ligament Reconstruction: Matched-Pair Design
- Preserving Remnant Tissue in Arthroscopic ACL Reconstruction Using Achilles Tendon Allograft
- Comparison of Magnetic Resonance Imaging of Remnant Preserving versus Remnant Sacrificing Technique after Anterior Cruciate Ligament Reconstruction; Clinical Results and Second-Look Arthroscopic Findings: Pilot Study
- Remnant-Preserving Anterior Cruciate Ligament Reconstruction Using a Three-Dimensional Fluoroscopic Navigation System