J Korean Soc Spine Surg.
2013 Sep;20(3):99-106. 10.4184/jkss.2013.20.3.99.
The Comparison of Clinical and Radiologic Results Classified by Translation Type and Fusion Method in the Isthmic Spondylolisthesis
- Affiliations
-
- 1Department of Orthopedic Surgery, College of Medicine, Dong-A University, Korea. gylee@dau.ac.kr
- KMID: 1487975
- DOI: http://doi.org/10.4184/jkss.2013.20.3.99
Abstract
- STUDY DESIGN: A retrospective study.
OBJECTIVES
To examine the radiologic and clinical results of patients classified as excessive translation and excessive angulation, treated by posterolateral fusion only, or posterolateral fusion with posterior lumbar interbody fusion in isthmic spondylolisthesis. SUMMARY OF LITERATURE REVIEW: Isthmic spondylolisthesis is usually treated by PLF only or PLF with PLIF. But it is not reported the clinical and radiologic results classified by translation type.
MATERIALS AND METHODS
Patients who had received surgery for spondylolisthesis between January 2005 to January 2010, there were 56 for whom follow-up observations were possible for 2 years. According to the fusion methods and preoperative flexion-extension simple radiograph, we classified as excessive translation and excessive angulation by segmental instability and as PLF and PLIF by surgical methods. We examine the clinical results(Visual Analogue Scale, Oswestry Distability Index, operation time, blood loss, complication rate) and the radiologic results(reduction rate of slippage, change of segmental angle, reduction ratio of disc height, bone union).
RESULTS
In radiologic results, excessive angulation(group II) did not show significant difference from excessive translation(group I) in terms of reduction rate of slippage, change of segmental angle, reduction ratio of disc height, bone union. But we found excessive translation-PLIF(group I-B) was better than excessive translation-PLF(group I-A) and excessive angulation-PLIF(group II-B) was better than excessive angulation-PLF(II-A) in terms of reduction ratio of disc height(P<0.05). In clinical results, both sides group did not show significant difference in operation time, blood loss, complication rate.
CONCLUSIONS
In spondylolisthesis patients, excessive translation group(I) and excessive angulation group(II) did not show significant difference in radiologic results and clinical results. But both sides group showed the PLF with PLIF was better than the PLF only in terms of reduction ratio of disc height.
Keyword
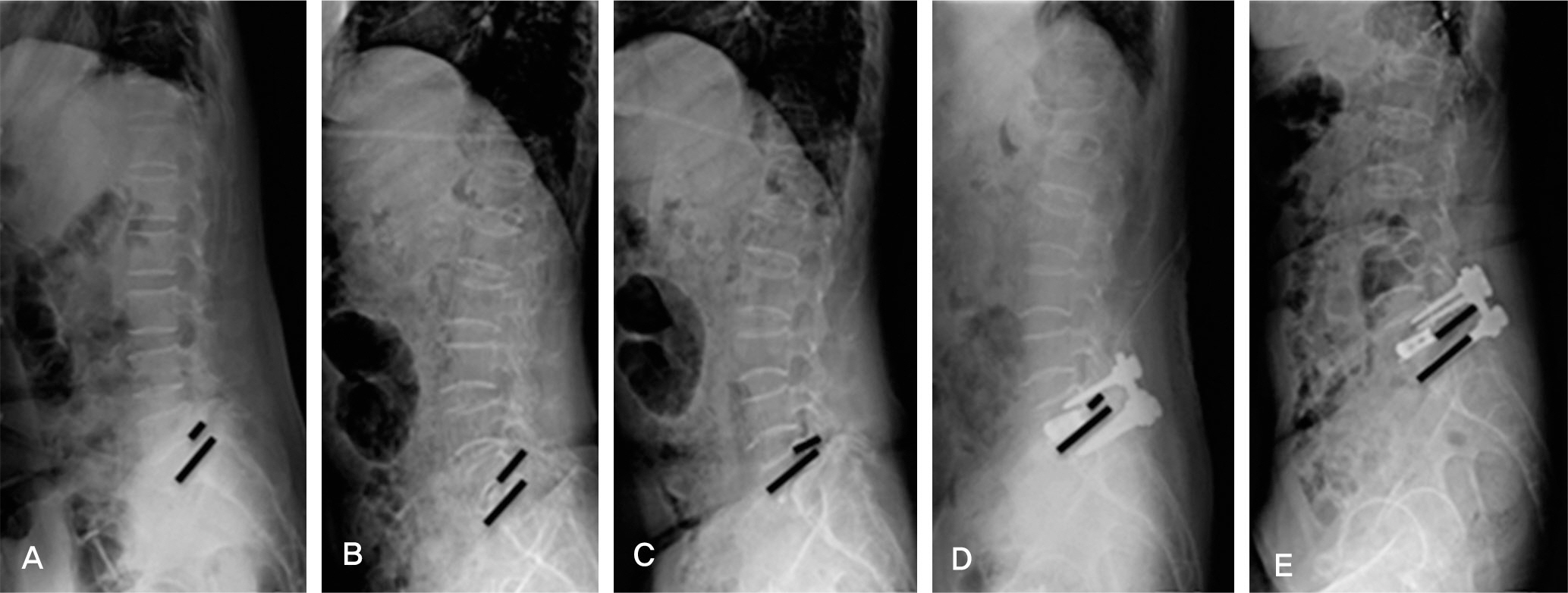
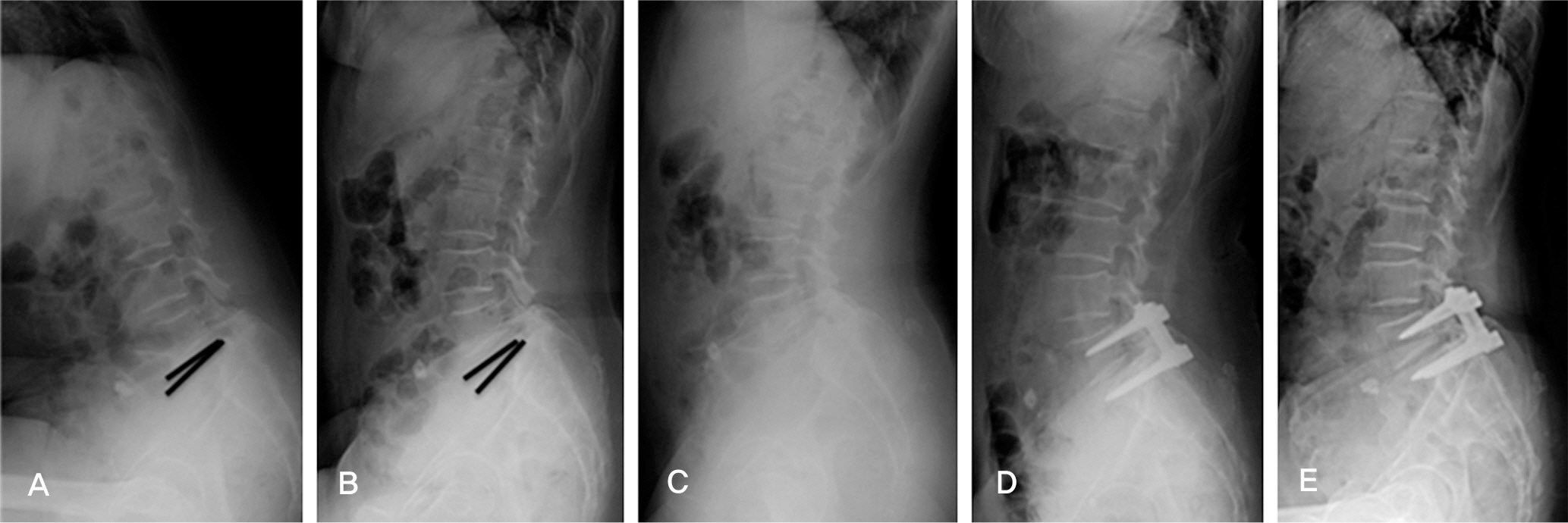
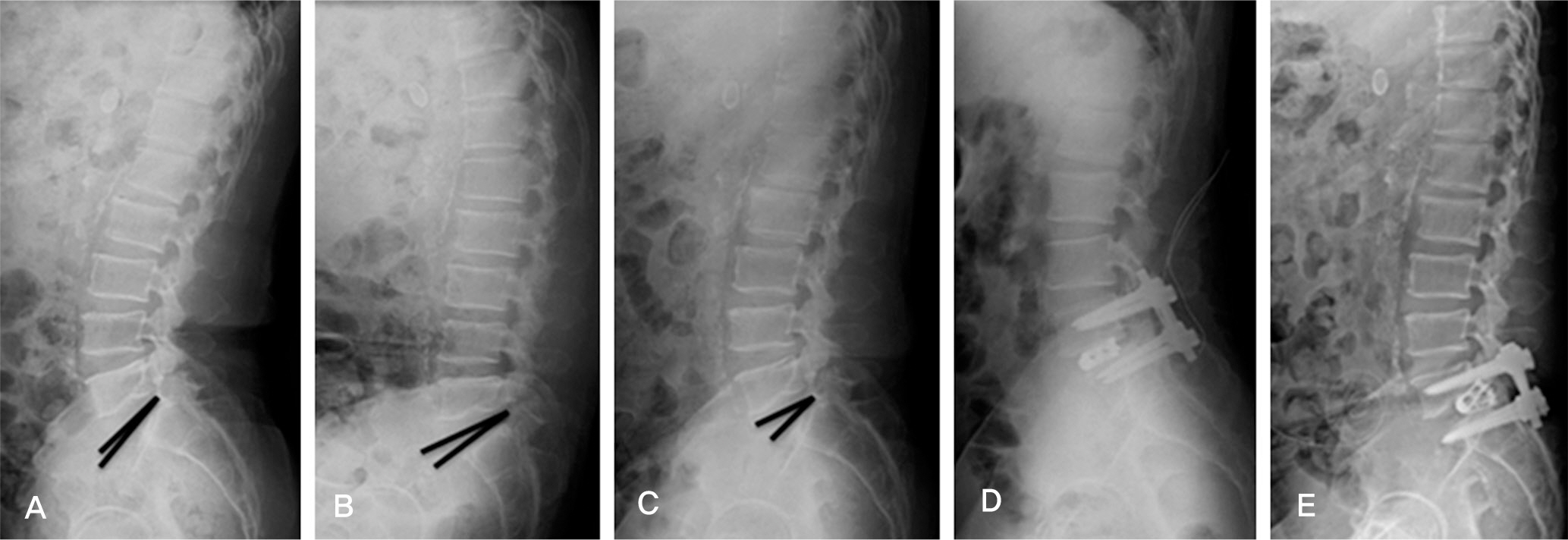
Figure
Reference
-
1. Wiltse LL, Newman PH, Macnab I. Classification of spondylolysis and spondylolisthesis. Clin Orthop. 1976; 117:23–9.2. Hu SS, Tribus CB, Diab M, Chanayem AJ. Spondylolisthesis and spondylolysis. J Bone Joint Surg Am. 2008; 90:656–91.3. Caputy A, Luessenhop A. Longterm evaluation of decompressive surgery for degenerative lumbar stenosis. J Neurosurg. 1992; 77:669–76.
Article4. Cauchoix J, Benoist M, Chassaing V. Degenerative spondylolisthesis. Clin Orthop Relat Res. 1976; 115:123–9.
Article5. Feffer H, Weisel S, Cuckler J, Rothman R. Degenerative spondylolisthesis: To fuse or not to fuse. Spine (Phila Pa 1976). 1985; 10:286–9.6. Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. J Bone Joint Surg. 1991; 73:802–7.7. Bridwell KG, Sedgewick TA, O’ Brien MF, Lenke LG, Baldus C. The role of fusion and instrumentation in the treatment of degenerative spondylolisthesis with spinal stenosis. J Spinal Disorder. 1993; 6:461–72.
Article8. Esses SI, Sach BL, Dreyzin V. Complications assocciated with the technique of pedicle screw fixations. Spine (Phila Pa 1976). 1993; 18:2231–9.9. Heim SE. Transpedicle instrumentation in the degenerative spine. Clin Orthop. 1997; 337:97–110.
Article10. Horowitch A, Peek RD, Thomas JC Jr, et al. The pedicle screw fixation system, early clinical results. Spine (Phila Pa 1976). 1989; 14:461–7.11. Suk SI, Lee CK, Kim WJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixatin and posterolateral fusion after decompression in spondylolytic spondylolisthesis. J Korean Orthop Assoc. 1995; 30:1638–46.
Article12. Wang JM, Kim DJ, Yun YH. Posterior pedicular screw instrumentation and anterior interbody fusion in adult lumbar spondylolysis or grade I spondyloilisthesis with segmental instability. J Spinal Disord. 1996; 9:83–8.13. Taillard W. [Spondylolisthesis in children and adolescents]. 1954; 24:115–44.15. Iguchi T, Kanemura A, Kasahara K, Kurihara A, Doita M, Yoshiya S. Age distribution of three radiologic factors for lumbar instability: probable aging process of the instability with disc degeneration. Spine (Phila Pa 1976). 2003; 28:2628–33.
Article16. Horowitch A, Peek RD, Thomas JC Jr, et al. The pedicle screw fixation system, early clinical results. Spine (Phila Pa 1976). 1989; 14:461–7.17. Kawakami M, Tamaki T, Ando M, Yamada H, Hashizume H, Yoshida M. Lumbar sagittal balance influences the clinical outcome after decompression and posterolateral spinal fusion for degenerative lumbar spondylolisthesis. Spine (Phila Pa 1976). 2002; 27:59–64.
Article18. Kim EH, Song IS. Additional posterior lumbar interbody fusion using threaded cage in spondylolisthesis with instability. J Korean Soc Spine Surg. 2000; 7:544–51.19. Madan S, Boeree NR. Outcome of posterior lumbar interbody fusion versus posterolateral fusion for spondylolytic spondylolisthesis. Spine (Phila Pa 1976). 2002; 27:1536–42.
Article20. Briggs H, Milligan PR. Chip fusion of the low back following exploration of the spinal canal. J Bone Joint Surg. 1994; 26:125–30.21. Cloward RB. Spondylolisthesis: treatment by laminectomy and posterior interbody fusion. Clin Orthop Relat Res. 1981; 154:74–82.22. Cloward RB. Posterior lumbar interbody fusion updated. Clin Orthop Relat Res. 1985; 193:16–9.
Article23. Ha KY, Moon MS, Rhyu KW, Song JH, Song HJ. Changes of fused segments after wide decompressive laminectomy and compact Cotrel-Dubousset instrumentation. J Korean Soc Spine Surg. 1996; 3:33–41.24. Enker P, Steffee AD. Interbody fusion and instrumentation. Clin Orthop Relat Res. 1994; 300:90–101.
Article25. Kim EH, Song IS. Additional posterior lumbar interbody fusion using threaded cage in spondylolisthesis with instability. J Korean Soc Spine Surg. 2000; 7:544–51.26. Suk SI, Lee CK, Kim WJ, Lee JH, Cho KJ, Kim HG. Adding posterior lumbar interbody fusion to pedicle screw fixation and posterolateral fusion after decompression in spondylolytic spondylolisthesis. Spine (Phila Pa 1976). 1997; 22:210–20.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of Surgical Treatment in Isthmic and Degenerative Spondylolisthesis
- MR Findings of Spondylolisthesis: Assessment of Associated Spinal and Neural Foraminal Stenosis
- Effect of Posterior Lumbar Interbody Fusion for Maintaining the Reduction in Isthmic Spondylolisthesis
- Comparison of Cinical Results between the Anterior Interbody Fusion and the Posterolateral Fusion with Transpedicular Fixation for the Treatment of Isthmic Spodylolisthesis in Adults
- Posterior Fixation and Interbody for Lumbar Spondylolisthesis