J Korean Fract Soc.
2010 Jan;23(1):90-96. 10.12671/jkfs.2010.23.1.90.
Reliability of the Radiographic Parameters in Pediatric Supracondylar Fracture
- Affiliations
-
- 1Department of Orthopaedic Surgery, Hallym University College of Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea.
- 2Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea. kunbopark@gmail.com
- KMID: 1461578
- DOI: http://doi.org/10.12671/jkfs.2010.23.1.90
Abstract
- PURPOSE
To suggest the most reliable guideline of the treatement for the supracondylar fracture in children by the comparison of the radiographic parameters between forearm supination-elbow extension and forearm pronation-elbow flexion view.
MATERIALS AND METHODS
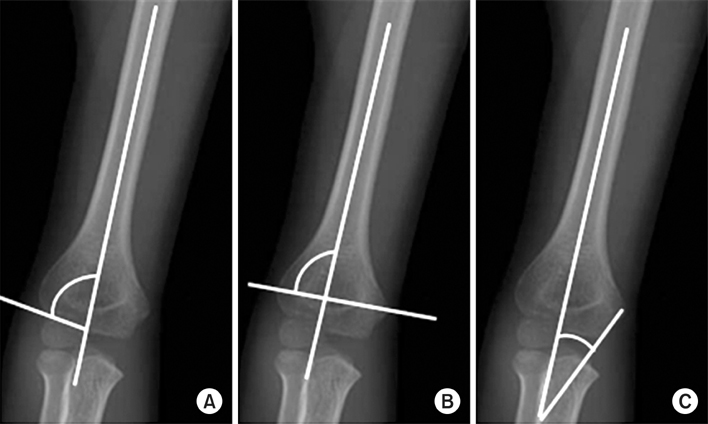
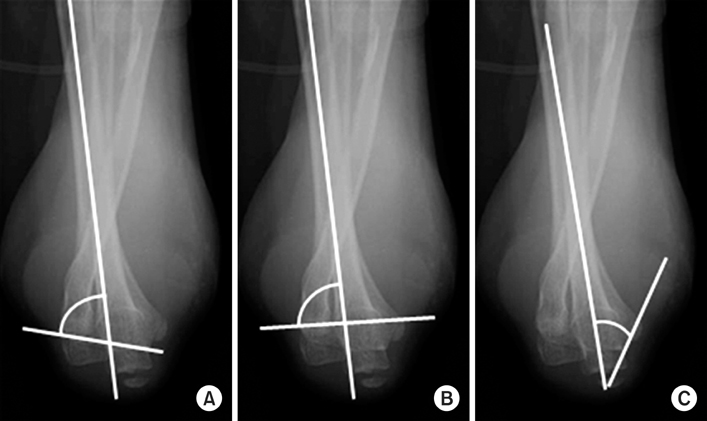
A total of seventy-one patients were included in the study. Baumann, metaphyseal diaphyseal and medial epicondylar epiphyseal angle of normal elbow in extension and flexion view were compared. Finally, the results of Group I (operation with elbow extension view) and Group II (operation with elbow flexion view) were compared.
RESULTS
Intraobserver reproducibility and interobserver reliability were better in the Baumann angle with extension view and metaphyseal diaphyseal angle with flexion view. In extension view, Baumann and metaphyseal diaphyseal angle show negative correlation with carrying angle but in flexion view, only metaphyseal diaphyseal angle shows negative correlation. Baumann angle were greater in flexion view and medial epicondylar epiphyseal angle were greater in extension view. There was no statistical difference in the final results of Group I and II.
CONCLUSION
Baumann angle was more effective in forearm supination-elbow extension view and metaphyseal diaphyseal angle was more effective in forearm pronation-elbow flexion view. The difference between elbow extension and flexion view should be considered during operation.
Keyword
Figure
Reference
-
1. Ariño VL, Lluch EE, Ramirez AM, Ferrer J, Rodriguez L, Baixauli F. Percutaneous fixation of supracondylar fractures of the humerus in children. J Bone Joint Surg Am. 1977. 59:914–916.
Article2. Biyani A, Gupta SP, Sharma JC. Determination of medial epicondylar epiphyseal angle for supracondylar humeral fractures in children. J Pediatr Orthop. 1993. 13:94–97.
Article3. Camp J, Ishizue K, Gomez M, Gelberman R, Akeson W. Alteration of Baumann's angle by humeral position: implications for treatment of supracondylar humerus fractures. J Pediatr Orthop. 1993. 13:521–525.4. Canale ST. Canale ST, editor. Fractures and dislocations in children. Campbell's operative orthopaedics. 1998. 10th ed. Philladelphia: Mosby Inc;1391–1565.
Article5. Cho HO, Kwak KD, Cho SD, Kim BY. Change in carrying angle after supracondylar fracture of the humerus in children. J Korean Soc Fract. 1994. 7:65–71.
Article6. Flynn JC, Matthews JG, Benoit RL. Blind pinning of displaced supracondylar fractures of the humerus in children Sixteen years' experience with long-term follow-up. J Bone Joint Surg Am. 1974. 56:263–272.
Article7. GARTLAND JJ. Management of supracondylar fractures of the humerus in children. Surg Gynecol Obstet. 1959. 109:145–154.8. Park SR, Kim HS, Kang JS, Lee WH, Kim SH. Assessments of reduction for supracondylar humerus fractures in children: comparison of clinical carrying angle, baumanns angle and metaphyseal-diaphyseal angle. J Korean Soc Fract. 1999. 12:660–666.
Article9. Kim ID, Lee SY, Kim PT, Park BC, Choi YW, Park SJ. Change of Carrying Angle in Fracture of the Lateral Humeral Condyle in Children. J Korean Orthop Assoc. 1987. 22:1257–1264.
Article10. Labelle H, Bunnell WP, Duhaime M, Poitras B. Cubitus varus deformity following supracondylar fractures of the humerus in children. J Pediatr Orthop. 1982. 2:539–546.
Article11. Lee SS, Mahar AT, Miesen D, Newton PO. Displaced pediatric supracondylar humerus fractures: biomechanical analysis of percutaneous pinning techniques. J Pediatr Orthop. 2002. 22:440–443.
Article12. Nacht JL, Ecker ML, Chung SM, Lotke PA, Das M. Supracondylar fractures of the humerus in children treated by closed reduction and percutaneous pinning. Clin Orthop Relat Res. 1983. 177:203–209.
Article13. Park DM, Lee JY, Kim KT, Sohn SK, Kim SS. Change of carrying angle in fracture of the lateral humeral condyle in children. J Korean Soc Fract. 1995. 8:140–151.
Article14. Shim JS, Lee YS. Treatment of completely displaced supracondylar fracture of the humerus in children by cross-fixation with three Kirschner wires. J Pediatr Orthop. 2002. 22:12–16.
Article15. Shrout PE, Fleiss JL. Intraclass correlations: uses in assessing rater reliability. Psychol Bull. 1979. 86:420–428.
Article16. Smith L. Deformity following supracondylar fractures of the humerus. J Bone Joint Surg Am. 1965. 47:1668.
Article17. Song YS, Yun SH. A study of the treatment and the measurements of carrying angle on the supracondylar fracture of the humerus in children. J Korean Soc Fract. 1997. 10:956–963.
Article18. Webb AJ, Sherman FC. Supracondylar fractures of the humerus in children. J Pediatr Orthop. 1989. 9:315–325.
Article19. Worlock P. Supracondylar fractures of the humerus. Assessment of cubitus varus by the Baumann angle. J Bone Joint Surg Br. 1986. 68:755–757.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Supracondylar Fracture of the Femur in Bowler
- Supracondylar Intramedullary Nail for Femoral Supracondylar Fracture following TKA: 3 Cases Report
- Radiologic Study of Torsion Type of Supracondylar Fracture of Humerus in Children
- Treatment of the Difficult Supracondylar Fracture of the Femur with the Intramedullary Supracondylar Nail
- Treatment of the Supracondylar Fractures of the Femur with an Interlocked Intramedullary Nail