Korean J Pediatr Gastroenterol Nutr.
2010 Sep;13(2):154-163. 10.5223/kjpgn.2010.13.2.154.
Clinical, Endoscopic and Pathologic Findings of Colonic Polyposis in Korean Children
- Affiliations
-
- 1Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea. jkseo@snu.ac.kr
- 2Department of Pathology, Seoul National University College of Medicine, Seoul, Korea.
- 3Department of Radiology, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 1459431
- DOI: http://doi.org/10.5223/kjpgn.2010.13.2.154
Abstract
- PURPOSE
Colonic polyposis is less common in children than in adults. The clinical data pertaining to colonic polyposis in children are limited. Children with colonic polyposis have complications associated with numerous polyps, malignant transformation of the polyps, and extraintestinal neoplasms. We studied the clinical spectrum, endoscopic characteristics, and histologic findings of colonic polyposis in Korean children.
METHODS
We reviewed the clinical data of 37 children with multiple colonic polyps between 1987 and 2009. The mean age at the time of diagnosis of colonic polyposis was 8.0+/-3.2 years.
RESULTS
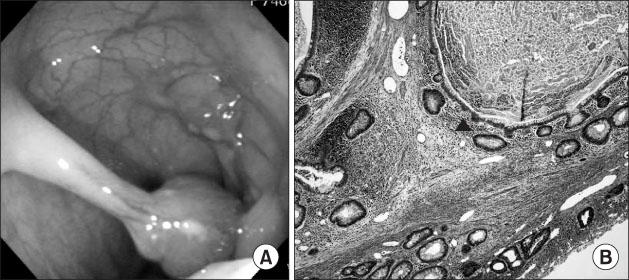
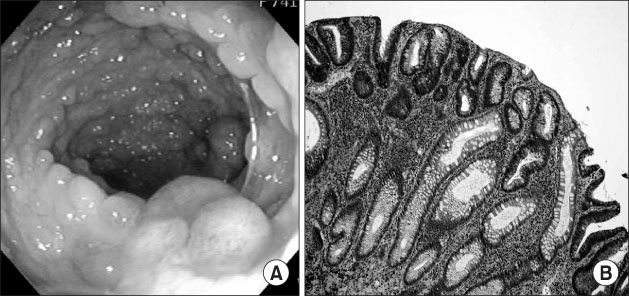
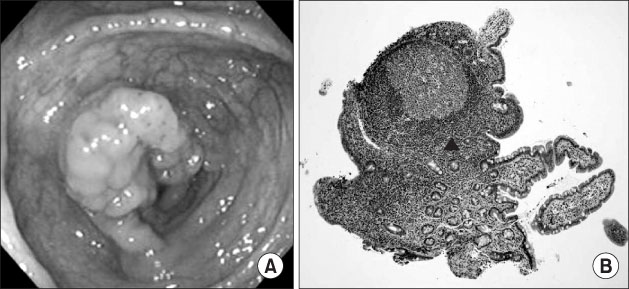
Peutz-Jeghers syndrome, juvenile polyposis syndrome, familial adenomatous polyposis (FAP), and lymphoid polyposis was diagnosed in 22, 7, 6, and 2 children, respectively. The most common clinical presentation in children with colonic polyposis was hematochezia. A family history of colonic polyposis was noted in 7 children. The colonoscopic findings of colonic polyposis varied with the size and number of polyps. The majority of polyps were multi-lobulatd and pedunculated in children with Peutz-Jeghers syndrome. The polyps in children with juvenile polyposis syndrome were primarily round and pedunculated. For the children with FAP, the colon was carpeted with small, sessile polyps. There were multiple sessile polyps in the patients with lymphoid polyposis. Surgical polypectomy was performed in 14 children (38%). Intestinal segmental resection was performed in 13 children (35%). Four patients with FAP underwent total colectomy. Four children with Peutz-Jeghers syndrome had extraintestinal neoplasms. No malignant transformation of polyp was identified.
CONCLUSION
Children with colonic polyposis should undergo a careful initial evaluation and require periodic re-evaluation.
Keyword
MeSH Terms
Figure
Cited by 3 articles
-
Incidentally Discovered Solitary Gastrointestinal Polyp with Pathological Significance in Children: Four Case Reports
Sang-eun Han, Jiyeon Chang, Seung Sam Paik, Yong Joo Kim
Pediatr Gastroenterol Hepatol Nutr. 2018;21(3):209-213. doi: 10.5223/pghn.2018.21.3.209.Juvenile Polyp associated with Hypovolemic Shock Due to Massive Lower Gastrointestinal Bleeding
Dong Yeop Kim, Joon Yeol Bae, Kyung Ok Ko, Eun Jung Cheon, Jae Woo Lim, Young Hwa Song, Jung Min Yoon
Pediatr Gastroenterol Hepatol Nutr. 2019;22(6):613-618. doi: 10.5223/pghn.2019.22.6.613.Peutz-Jeghers Syndrome with Adenomatous Change in a Fifteen-month-old Boy
Kun Song Lee, Seung Ho Lee, Na-Hye Myong
Korean J Gastroenterol. 2015;66(2):106-110. doi: 10.4166/kjg.2015.66.2.106.
Reference
-
1. Kim SJ, Kim SM, Kim YJ, Jeong DC, Lee WB, Chung SY, et al. Colonic polyps; experience of 34 cases in two hospitals. Korean J Pediatr. 2004. 47:756–761.2. Gelb AM, Minkowitz S, Tresser M. Rectal and colonic polyps occurring in young people. N Y State J Med. 1962. 62:513–518.3. Mestre JR. The changing pattern of juvenile polyps. Am J Gastroenterol. 1986. 81:312–314.4. Poddar U, Thapa BR, Vaiphei K, Singh K. Colonic polyps: experience of 236 Indian children. Am J Gastroenterol. 1998. 93:619–622.
Article5. Durno CA. Colonic polyps in children and adolescents. Can J Gastroenterol. 2007. 21:233–239.
Article6. Latt TT, Nicholl R, Domizio P, Walker-Smith JA, Williams CB. Rectal bleeding and polyps. Arch Dis Child. 1993. 69:144–147.
Article7. Longo WE, Touloukian RJ, West AB, Ballantyne GH. Malignant potential of juvenile polyposis coli. Report of a case and review of the literature. Dis Colon Rectum. 1990. 33:980–984.8. Goh PG, Moon HS, Sung JK, Jeong HY, Song KS. A case of Peutz-Jeghers syndrome with intraductal papillary mucinous carcinoma of pancreas. Korean J Gastroenterol. 2010. 55:73–77.
Article9. Kim JO, Kong HP, Park KS, Kim WS, Lee CH. A case of nonfamilial generalized gastrointestinal juvenile polyposis with pancytopenia. J Korean Pediatr Soc. 1996. 39:423–430.10. Kwak JW, Kim HY, Park JH. Polypectomy by intraoperative total gut endoscopy in a child with Peutz-Jeghers syndrome. Korean J Pediatr Gastroenterol Nutr. 2005. 8:76–80.
Article11. Jean-Francois M, Sylviane O, Michel P. Walker WA, Walker SJ, editors. Pediatric gastrointestinal disease. Intestinal polyps and polyposis. 2008. 5th ed. Hamilton: BC Decker Inc;637–652.12. Elitsur Y, Teitelbaum JE, Rewalt M, Nowicki M. Clinical and endoscopic data in juvenile polyposis syndrome in preadolescent children: a multicenter experience from the United States. J Clin Gastroenterol. 2009. 43:734–736.
Article13. Kang BY, Han SJ, Lee JE, Choi SK, Kim JM, Hong YJ, et al. A case of juvenile polyposis presented with protein losing enteropathy. Korean J Pediatr Gastroenterol Nutr. 2003. 6:208–214.
Article14. Chang MS, Kim YI. Intestinal polyposis: a clinicopathologic analysis of 28 resected cases with special reference to surgical intervention. Korean J Gastroenterol. 1991. 23:62–74.15. Farmer RG, Hawk WA, Turnbull RB Jr. The spectrum of the Peutz-Jeghers syndrome. Report of 3 cases. Am J Dig Dis. 1963. 8:953–961.16. Calva D, Howe JR. Hamartomatous polyposis syndromes. Surg Clin North Am. 2008. 88:779–817.
Article17. Jass JR. Colorectal polyposes: from phenotype to diagnosis. Pathol Res Pract. 2008. 204:431–447.
Article18. Kojima M, Itoh H, Motegi A, Sakata N, Masawa N. Localized lymphoid hyperplasia of the rectum resembling polypoid mucosa-associated lymphoid tissue lymphoma: a report of three cases. Pathol Res Pract. 2005. 201:757–761.
Article19. Seo JK. Therapeutic colonoscopy in children: endoscopic snare polypectomy and juvenile polyps. Seoul J Med. 1993. 34:285–294.20. Howe JR, Ringold JC, Hughes JH, Summers RW. Direct genetic testing for SMAD4 mutations in patients at risk for juvenile polyposis. Surgery. 1999. 126:162–170.
Article21. Schmid C, Vazquez JJ, Diss TC, Isaacson PG. Primary B-cell mucosa-associated lymphoid tissue lymphoma presenting as a solitary colorectal polyp. Histopathology. 1994. 24:357–362.
Article22. Byrne WJ, Jimenez JF, Euler AR, Golladay ES. Lymphoid polyps (focal lymphoid hyperplasia) of the colon in children. Pediatrics. 1982. 69:598–600.
Article23. Scully RE. Sex cord tumor with annular tubules a distinctive ovarian tumor of the Peutz-Jeghers syndrome. Cancer. 1970. 25:1107–1121.
Article24. Van Lier MG, Wagner A, Mathus-Vliegen EM, Kuipers EJ, Steyerberg EW, Van Leerdam ME. High cancer risk in Peutz-Jeghers syndrome: a systematic review and surveillance recommendations. Am J Gastroenterol. 2010. 105:1258–1264.
Article25. Barnard J. Screening and surveillance recommendations for pediatric gastrointestinal polyposis syndromes. J Pediatr Gastroenterol Nutr. 2009. 48:Suppl 2. S75–S78.
Article26. Attard TM, Young RJ. Diagnosis and management of gastrointestinal polyps: pediatric considerations. Gastroenterol Nurs. 2006. 29:16–22. quiz 3-4.27. Park JG, Kim IJ. Hereditary colorectal cancer. Korean J Gastroenterol. 2005. 45:78–87.28. Vasen HF, Moslein G, Alonso A, Aretz S, Bernstein I, Bertario L, et al. Guidelines for the clinical management of familial adenomatous polyposis (FAP). Gut. 2008. 57:704–713.
Article29. Merg A, Howe JR. Genetic conditions associated with intestinal juvenile polyps. Am J Med Genet C Semin Med Genet. 2004. 129C:44–55.
Article30. Volikos E, Robinson J, Aittomaki K, Mecklin JP, Jarvinen H, Westerman AM, et al. LKB1 exonic and whole gene deletions are a common cause of Peutz-Jeghers syndrome. J Med Genet. 2006. 43:e18.
Article31. Yang HR, Ko JS, Seo JK. Germline mutation analysis of STK11 gene using direct sequencing and multiplex ligation-dependent probe amplification assay in Korean children with Peutz-Jeghers syndrome. Dig Dis Sci. 2010.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Gastric Hyperplastic Polyposis Associated with Colonic Hyperplastic Polyposis
- Is Colonoscopy Necessary in Children Suspected of Having Colonic Polyps?
- Familial Adenomatous Polyposis: Two cases
- A Case of Gastric and Colonic Hyperplastic Polyposis Associated with Colonic Adenomas
- Familial Polyposis Coli