J Korean Hip Soc.
2011 Dec;23(4):282-289. 10.5371/jkhs.2011.23.4.282.
Isolated Polyethylene Liner Exchange in a Revision Total Hip Arthroplasty
- Affiliations
-
- 1Department of Orthopaedic Surgery, College of Medicine, Kyung Hee University, Seoul, Korea. yjcho@khmc.or.kr
- KMID: 1452636
- DOI: http://doi.org/10.5371/jkhs.2011.23.4.282
Abstract
- PURPOSE
To analyze the results of isolated exchange of polyethylene (PE) liners for treatment of wear and osteolysis around a well-fixed Harris-Galante (HG) cementless acetabular cup.
MATERIALS AND METHODS
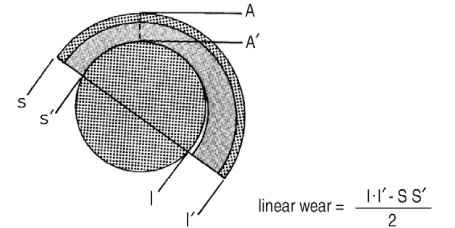
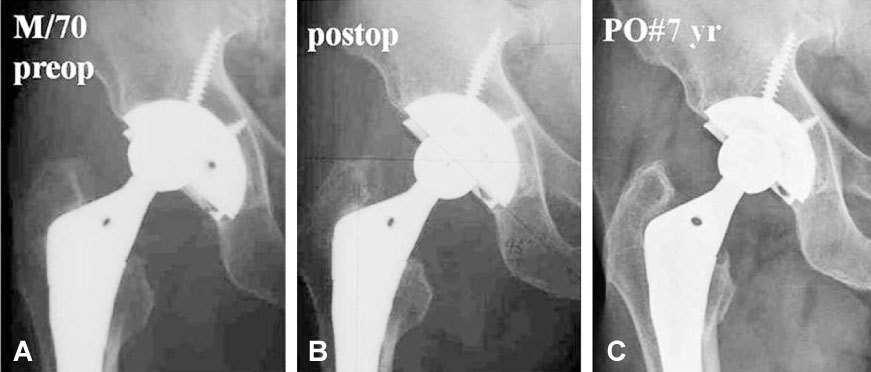
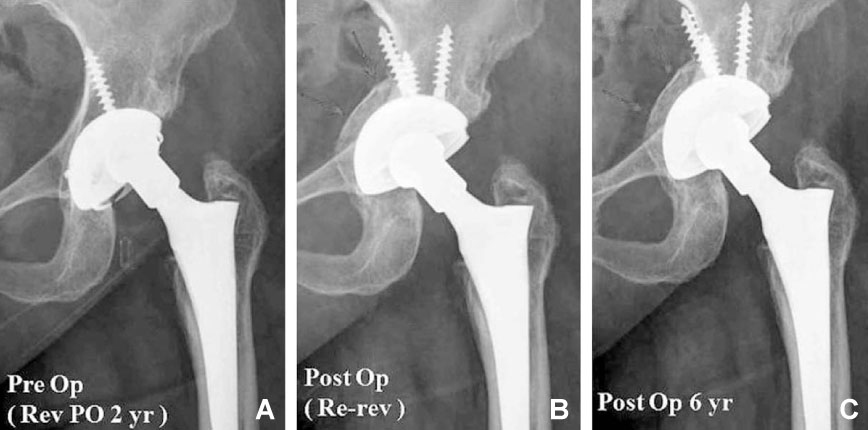
Thirty-three PE liner changes were performed without the removal of stably ingrown implants (33 hips of 32 patients). They were able to be followed for a mean period of 92 months. Clinically, the Harris hip score (HHS), pain evaluation, and complications were evaluated. Radiologically, the annual wear rate and the size of the osteolytic lesions were measured before the operation and the latest follow-up. The bone graft incorporation scale and the development of new osleolytic lesions were checked during the final follow-up.
RESULTS
HHS improved to 89.3 at last follow-up. The size of the osteolysis was significantly reduced postoperatively. Bone graft incorporation scales were Grade I in 9 and Grade II in 14 cases. New osteolytic lesions have not developed at latest follow-up. As a complication, one case of dissociation of a liner and a periprosthetic fracture were noted. Annual wear rates during the same period were significantly reduced. There was no sign of alteration in stability of the PE liner.
CONCLUSION
Exchange of a PE liner without removal of stable implants can be a good option for the treatment of wear and osteolysis around a stable cementless THA implant, even if the system has a weak locking mechanism, such as the HG cup. In these cases, under certain states with a higher risk of early failure in the locking mechanism, it would be better to select other revision procedures such as cup revision or cemented polyethylene liner fixation.
Keyword
MeSH Terms
Figure
Reference
-
1. Berry DJ. Management of osteolysis around total hip arthroplasty. Orthopedics. 1999. 22:805–808.
Article2. D'Antonio JA, Capello WN, Borden LS, et al. Classification and management of acetabular abnormalities in total hip arthroplasty. Clin Orthop Relat Res. 1989. 243:126–137.3. O'Brien DA, Rorabeck CH. Managing bone loss in revision total hip arthroplasty: the aetabulum. Instr Course Lect. 2006. 55:263–277.4. Benson ER, Christensen CP, Monesmith EA, Gomes SL, Bierbaum BE. Particulate bone grafting of osteolytic femoral lesions around stable cementless stems. Clin Orthop Relat Res. 2000. 381:58–67.
Article5. Maloney WJ, Herzwurm P, Paprosky W, Rubash HE, Engh CA. Treatment of pelvic osteolysis associated with a stable acetabular component inserted without cement as part of a total hip replacement. J Bone Joint Surg Am. 1997. 79:1628–1634.
Article6. Paprosky WG, Perona PG, Lawrence JM. Acetabular defect classification and surgical reconstruction in revision arthroplasty. A 6-year follow-up evaluation. J Arthroplasty. 1994. 9:33–44.
Article7. Rubash HE, Sinha RK, Maloney WJ, Paprosky WG. Osteolysis: surgical treatment. Instr Course Lect. 1998. 47:321–329.8. Dorr LD, Wan Z, Gruen T. Functional results in total hip replacement in patients 65 years and older. Clin Orthop Relat Res. 1997. 336:143–151.
Article9. Hozack WJ, Bicalho PS, Eng K. Treatment of femoral osteolysis with cementless total hip revision. J Arthroplasty. 1996. 11:668–672.
Article10. Schmalzried TP, Fowble VA, Amstutz HC. The fate of pelvic osteolysis after reoperation. No recurrence with lesional treatment. Clin Orthop Relat Res. 1998. 350:128–137.
Article11. DeLee JG, Charnley J. Radiological demarcation of cemented sockets in total hip replacement. Clin Orthop Relat Res. 1976. 121:20–32.
Article12. Kim HJ, Lee JH, Oh HC, Kim YM, Kim SR. A comparision of osteolysis in bipolar hemiarthroplasty and total hip arthroplasty. J Korean Orthop Assoc. 2000. 35:83–88.
Article13. Maloney WJ, Peters P, Engh CA, Chandler H. Severe osteolysis of the pelvic in association with acetabular replacement without cement. J Bone Joint Surg Am. 1993. 75:1627–1635.
Article14. Schmalzried TP, Guttmann D, Grecula M, Amstutz HC. The relationship between the design, position, and articular wear of acetabular components inserted without cement and the development of pelvic osteolysis. J Bone Joint Surg Am. 1994. 76:677–688.
Article15. Lie SA, Hallan G, Furnes O, Havelin LI, Engesaeter LB. Isolated acetabular liner exchange compared with complete acetabular component revision in revision of primary uncemented acetabular components: a study of 1649 revisions from the Norwegian Arthroplasty Register. J Bone Joint Surg Br. 2007. 89:591–594.16. Clohisy JC, Harris WM. The Harris-Galante porous-coated acetabular component with screw fixation. An average ten-year follow-up study. J Bone Joint Surg Am. 1999. 81:66–73.
Article17. González della Valle A, Ruzo PS, Li S, Pellicci P, Sculco TP, Salvati EA. Dislodgment of polyethylene liners in first and second-generation Harris-Galante acetabular components. A report of eighteen cases. J Bone Joint Surg Am. 2001. 83-A:553–559.18. Lachiewicz PF, Soileau ES. Polyethylene liner exchange of the Harris-Galante porous I and II acetabular components without cement: results and complications. J Arthroplasty. 2006. 21:992–997.
Article19. Röhrl SM, Nivbrant B, Snorrason F, Kärrholm J, Nilsson KG. Porous-coated cups fixed with screws: a 12-year clinical and radiostereometric follow-up study of 50 hips. Acta Orthop. 2006. 77:393–401.
Article20. Talmo CT, Kwon YM, Freiberg AA, Rubash HE, Malchau H. Management of polyethylene wear associated with a well-fixed modular cementless shell during revision total hip arthroplasty. J Arthroplasty. 2011. 26:576–581.
Article21. Rubash HE, Sinha RK, Paprosky W, Engh CA, Maloney WJ. A new classification system for the management of acetabular osteolysis after total hip arthroplasty. Instr Course Lect. 1999. 48:37–42.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ceramic Head Fracture in Ceramic-on-Polyethylene Total Hip Arthroplasty
- Failure of a Metal Femoral Head after Revision Total Hip Arthroplasty for a Ceramic Liner Fracture
- Exchange and Reorientation of an Elevated-rim Polyethylene Liner for the Recurrent Anterior Subluxation after Total Hip Arthroplasty: A Case Report
- Finite Element Analysis of Stress Distribution in Flat and Elevated-Rim Polyethylene Acetabular Liners
- An Inguinal Mass associated with Polyethylene Wear Debris after a Total Hip Arthroplasty: A Case Report