J Korean Assoc Oral Maxillofac Surg.
2011 Aug;37(4):295-300. 10.5125/jkaoms.2011.37.4.295.
Experimental study about the bony healing of hydroxyapatite coating implants
- Affiliations
-
- 1Interdisciplinary Program in Biomedical, Pusan National University, Busan, Korea.
- 2Implant R&D Center, OSSTEM IMPLANT Co., Ltd., Busan, Korea.
- 3Department of Oral and Maxillofacial Surgery, Section of Dentistry, Seoul National University Bundang Hospital, School of Dentistry, Seoul National University, Seongnam, Korea. kyk0505@snubh.org
- 4Pusan National University, School of Dentistry, Busan, Korea.
- 5Apsun Dental Hospital, Seoul, Korea.
- KMID: 1449062
- DOI: http://doi.org/10.5125/jkaoms.2011.37.4.295
Abstract
- INTRODUCTION
Hydroxyapatite(HA) coating implant can accelerate osseointegration, however, there are many controversies.
MATERIALS AND METHODS
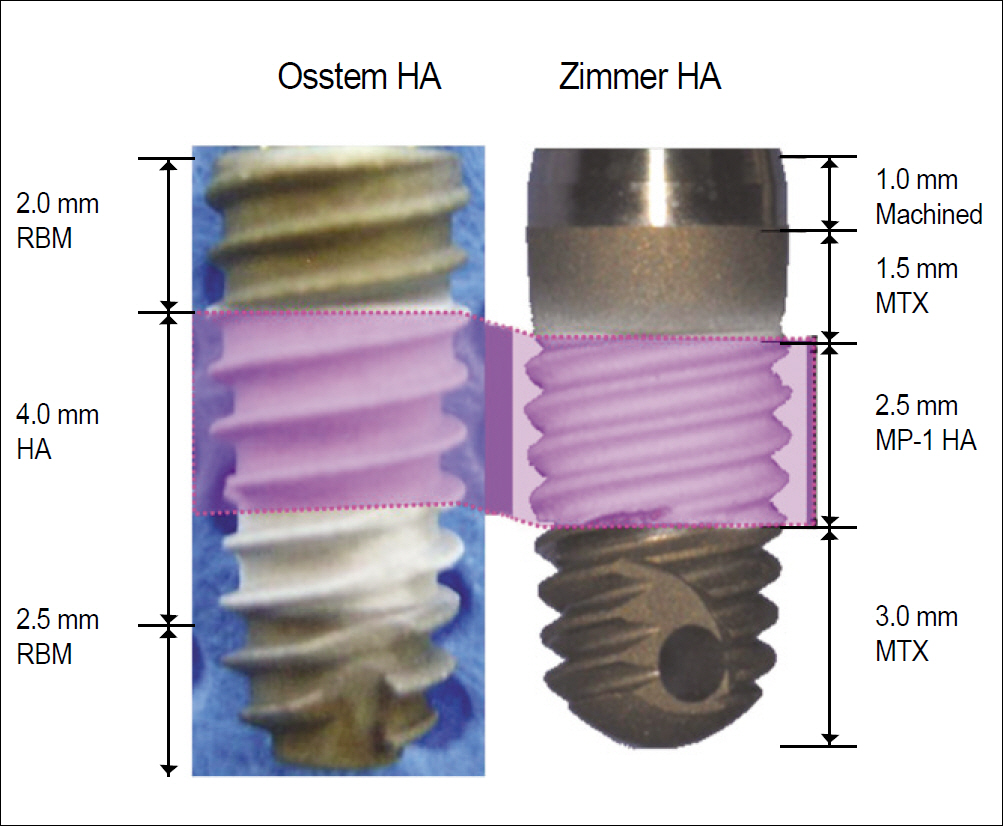
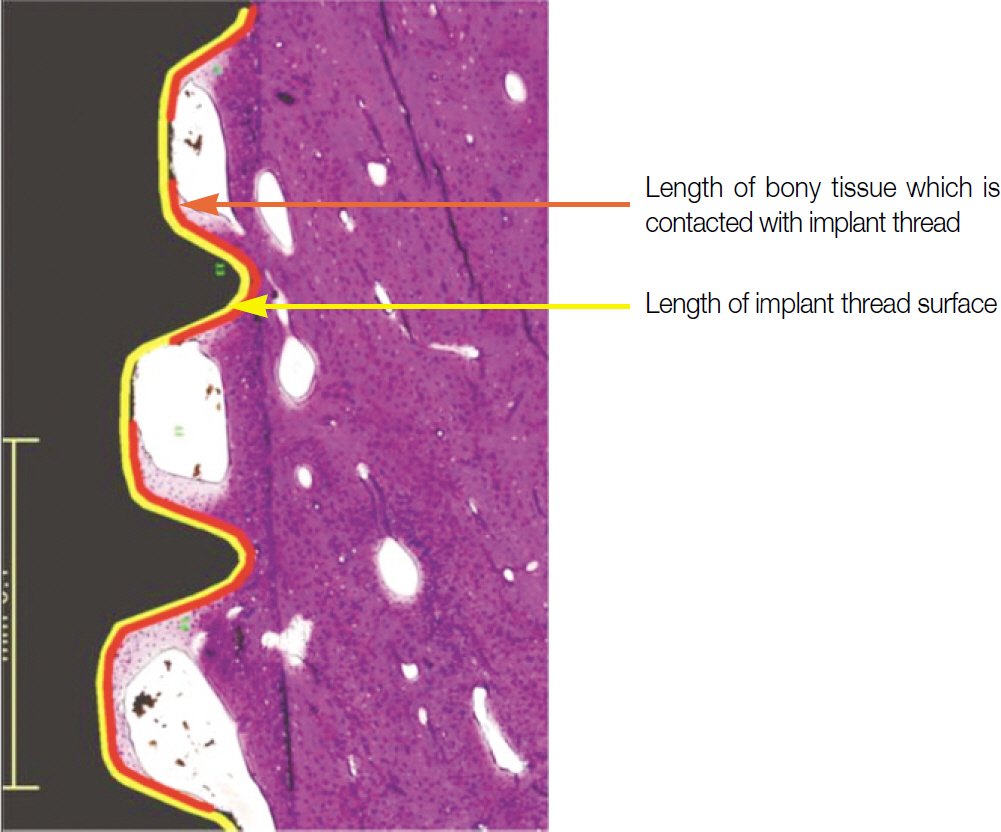
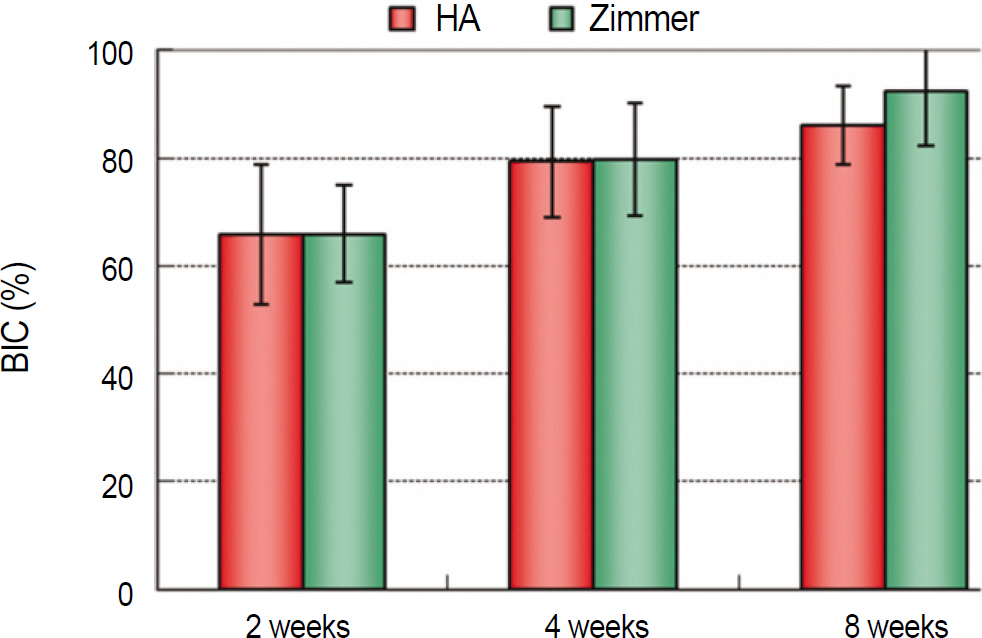
This study examined the early osseointegration of two types of hydroxyapatite coated implants. Twelve adult male miniature pigs (Medi Kinetics Micropigs, Medi Kinetics Co., Ltd., Busan, Korea) were used in this study. In the implants placed in the mandible, a histomorphometric evaluation was performed to evaluate the bone-implant contact (BIC) ratio.
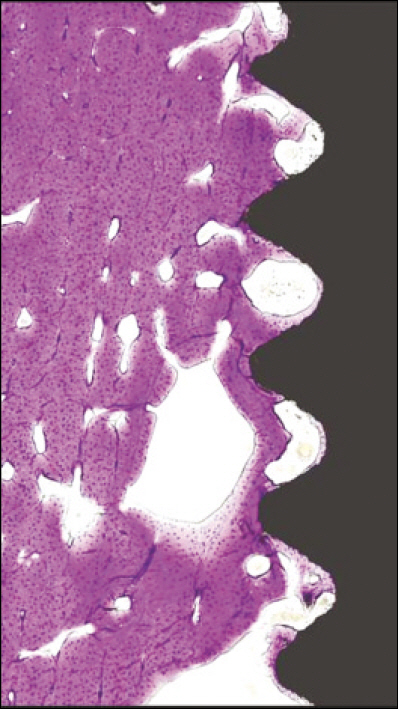
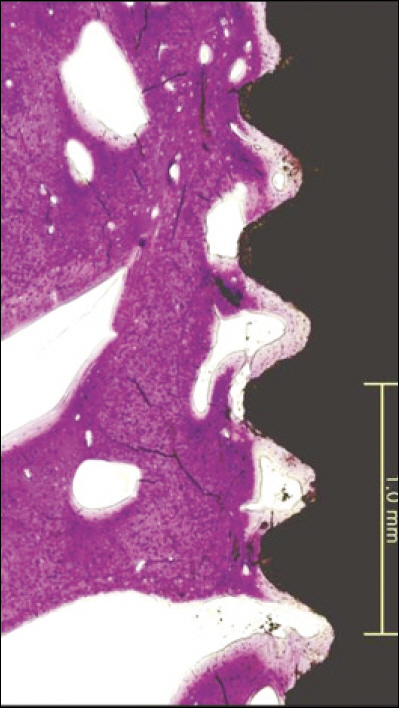
RESULTS
The BIC ratio increased with time. TS III HA and Zimmer HA were not significantly different (P>0.05). At 8 weeks, the BIC of Zimmer HA was higher than TS III HA, but there was no significant difference (P>0.05).
CONCLUSION
HA coated implants will accelerate early osseointegration.
MeSH Terms
Figure
Cited by 1 articles
-
Hydroxyapatite-coated implant: Clinical prognosis assessment via a retrospective follow-up study for the average of 3 years
Jun-Hong Jung, Sang-Yun Kim, Yang-Jin Yi, Bu-Kyu Lee, Young-Kyun Kim
J Adv Prosthodont. 2018;10(2):85-92. doi: 10.4047/jap.2018.10.2.85.
Reference
-
1. Jeong R, Marin C, Granato R, Suzuki M, Gil JN, Granjeiro JM, et al. Early bone healing around implant surfaces treated with variations in the resorbable blasting media method. A study in rabbits. Med Oral Patol Oral Cir Bucal. 2010; 15(1):e119–25.
Article2. Abdel-Haq J, Karabuda CZ, Arısan V, Mutlu Z, Körkçö M. Osseointegration and stability of a modified sand-blasted acid-etched implant: an experimental pilot study in sheep. Clin Oral Implants. 2011; 22:265–74.
Article3. Zhu X, Ong JL, Kim S, Kim K. Surface characteristics and structure of anodic oxide films containing Ca and P on a titanium implant material. J Biomed Mater Res. 2002; 60:333–8.
Article4. Whitehead RY, Lucas LC, Lacefield WR. The effect of dissolution on plasma sprayed hydroxylapatite coatings on titanium. Clin Mater. 1993; 12:31–9.
Article5. Wheeler SL. Eight-year clinical retrospective study of titanium plasma-sprayed and hydroxyapatite-coated cylinder implants. Int J Oral Maxillofac Implants. 1996; 11:340–50.
Article6. Trisi P, Keith DJ, Rocco S. Human histologic and histomorphometric analyses of hydroxyapatite-coated implants after 10 years of unction: a case report. Int J Oral Maxillofac Implants. 2005; 20:124–30.7. McGlumphy EA, Peterson LJ, Larsen PE, Jeffcoat MK. Prospective study of 429 hydroxyapatite-coated cylindric om-niloc implants placed in 121 patients. Int J Oral Maxillofac Implants. 2003; 18:82–92.8. Lee JJ, Rouhfar L, Beirne OR. Survival of hydroxyapatite-coated implants: a meta-analytic review. J Oral Maxillofac Surg. 2000; 58:1372–9.
Article9. Morris HF, Ochi S. Hydroxyapatite-coated implants: a case for their use. J Oral Maxillofac Surg. 1998; 56:1303–11.
Article10. Chang YL, Lew D, Park JB, Keller JC. Biomechanical and morphometric analysis of hydroxyapatite-coated implants with varying crystallinity. J Oral Maxillofac Surg. 1999; 57:1096–108.11. Kim H, Choi SH, Chung SM, Li LH, Lee IS. Enhanced bone forming ability of SLA-treated Ti coated with a calcium phosphate thin film formed by e-beam evaporation. Biomed Mater. 2010; 5:044106.
Article12. Rohner D, Tay A, Chung SM, Hutmacher DW. Interface of unloaded titanium implants in the iliac crest, fibula, and scapula: a histomorphometric and biomechanical study in the pig. Int J Oral Maxillofac Implants. 2004; 19:52–8.13. Choi JY, Jung UW, Lee IS, Kim CS, Lee YK, Choi SH. Resolution of surgically created three-wall intrabony defects in implants using three different biomaterials: an in vivo study. Clin Oral Implants Res. 2011; 22:343–8.14. Thierer T, Davliakos JP, Keith JD Jr, Sanders JJ, Tarnow DP, Rivers JA. Five-year prospective clinical evaluation of highly crystalline HA MP-1-coated dental implants. J Oral Implantol. 2008; 34:39–46.
Article15. Artzi Z, Carmeli G, Kozlovsky A. A distinguishable observation between survival and success rate outcome of hydroxyapatite-coated implants in 5-10 years in function. Clin Oral Implants Res. 2006; 17:85–93.
Article16. Osstem Implant Co. TS III HA implant system clinical monitoring. 2010. 1–36. Busan.17. Cook SD, Key JF, Thomas KA, Jarcho M. Interface mechanics and histology of titanium and hydroxylapatite-coated titanium for dental implant applications. Int J Oral Maxillofac Implants. 1987; 2:15–22.18. Block MS, Kent JN, Kay JF. Evaluation of hydroxylapatite-coated titanium dental implants in dogs. J Oral Maxillofac Surg. 1987; 45:601–7.
Article19. Baker D, London RM, O’ Neal R. Rate of pull-out strength gain of dual-etched titanium implants: a comparative study in rabbits. Int J Oral Maxillofac Implants. 1999; 14:722–8.20. Friberg B, Sennerby L, Linden B, Grondahl K, Lekholm U. Stability measurements of one-stage Brånemark implants during healing in mandibles. A clinical resonance frequency analysis study. Int J Oral Maxillofac Surg. 1999; 28:266–72.21. Noguerol B, Mun ̃oz R, Mesa F, de Dios Luna J, O’ Valle F. Early implant failure. Prognostic capacity of Periotest: retrospective study of a large sample. Clin Oral Implants Res. 2006; 17:459–64.22. Masuda T, Yliheikkilä PK, Felton DA, Cooper LF. Generalizations regarding the process and phenomenon of osseointegration. Part I. In vivo studies. Int J Oral Maxillofac Implants. 1998; 13:17–29.23. Nkenke E, Fenner M, Vairaktaris EG, Neukam FW, Radespiel-Tröger M. Immediate versus delayed loading of dental implants in the maxillae of minipigs. Part II: histomorphometric analysis. Int J Oral Maxillofac Implants. 2005; 20:540–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Cementless Total Hip Arthroplasty Using Hydroxyapatite-Coated Femoral stem. - Two-Year Clinical and Radiologic Follow-UP-
- Teh Effect of Hydroxyapatite Coating on the Mechanical Strengths and Histologic Profiles of Porous Titanium Implants in Dogs
- The effects of Hydroxyapatite nano-coating implants on healing of surgically created circumferential gap in dogs
- Comparative study for osseointegration according to surface treatments of dental implants
- Experimental Study of Osseointegration and Stability of Intentionally Exposed Hydroxyapatite Coating Implants