J Korean Surg Soc.
2011 Dec;81(6):423-426. 10.4174/jkss.2011.81.6.423.
Gallbladder pseudolithiasis caused by ceftriaxone in young adult
- Affiliations
-
- 1Department of Surgery, The Armed Forces Gangneung Hospital, Gangneung, Korea.
- 2Department of Internal Medicine, The Armed Forces Gangneung Hospital, Gangneung, Korea.
- 3Department of Radiology, The Armed Forces Capital Hospital, Seongnam, Korea.
- 4Department of Internal Medicine, The Armed Forces Pusan Hospital, Busan, Korea.
- 5Department of Surgery, Soonchunhyang University College of Medicine, Seoul, Korea. hurusa@hanmail.net
- KMID: 1445773
- DOI: http://doi.org/10.4174/jkss.2011.81.6.423
Abstract
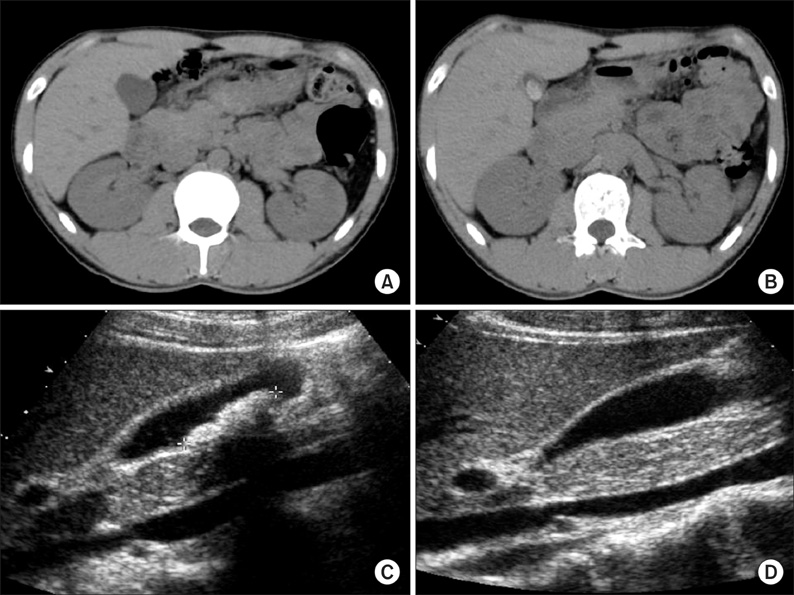
- Ceftriaxone is a commonly used antibiotic due to some of its advantages. Reversible gallbladder (GB) sludge or stone has been reported after ceftriaxone therapy. Most of these patients have no symptom, but the GB sludge or stone can sometimes cause cholecystitis. We experienced two patients who had newly developed GB stones after ceftriaxone therapy for diverticulitis and pneumonia, and this resolved spontaneously 1 month after discontinuation of the drug. Awareness of this complication could help to prevent unnecessary cholecystectomy.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Clinical Review and Case Report of Ceftriaxone-associated Gallbladder Pseudolithiasis in Adult
Hwa Kyung Jung, Dong-Shik Lee
Korean J Gastroenterol. 2014;63(6):378-381. doi: 10.4166/kjg.2014.63.6.378.
Reference
-
1. Biner B, Oner N, Celtik C, Bostancioğlu M, Tunçbilek N, Güzel A, et al. Ceftriaxone-associated biliary pseudolithiasis in children. J Clin Ultrasound. 2006. 34:217–222.2. Schaad UB, Wedgwood-Krucko J, Tschaeppeler H. Reversible ceftriaxone-associated biliary pseudolithiasis in children. Lancet. 1988. 2:1411–1413.3. Prince JS, Senac MO Jr. Ceftriaxone-associated nephrolithiasis and biliary pseudolithiasis in a child. Pediatr Radiol. 2003. 33:648–651.4. Richards DM, Heel RC, Brogden RN, Speight TM, Avery GS. Ceftriaxone. A review of its antibacterial activity, pharmacological properties and therapeutic use. Drugs. 1984. 27:469–527.5. Park HZ, Lee SP, Schy AL. Ceftriaxone-associated gallbladder sludge. Identification of calcium-ceftriaxone salt as a major component of gallbladder precipitate. Gastroenterology. 1991. 100:1665–1670.6. Arpacik M, Ceran C, Kaya T, Karadas B, Sarac B, Koyluoğlu G. Effects of ceftriaxone sodium on in vitro gallbladder contractility in guinea pigs. J Surg Res. 2004. 122:157–161.7. Shiffman ML, Keith FB, Moore EW. Pathogenesis of ceftriaxone-associated biliary sludge. In vitro studies of calcium-ceftriaxone binding and solubility. Gastroenterology. 1990. 99:1772–1778.8. Becker CD, Fischer RA. Acute cholecystitis caused by ceftriaxone stones in an adult. Case Report Med. 2009. 2009:132452.9. Lee SP, Lipsky BA, Teefey SA. Gallbladder sludge and antibiotics. Pediatr Infect Dis J. 1990. 9:422–423.10. Schaad UB, Suter S, Gianella-Borradori A, Pfenninger J, Auckenthaler R, Bernath O, et al. A comparison of ceftriaxone and cefuroxime for the treatment of bacterial meningitis in children. N Engl J Med. 1990. 322:141–147.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ceftriaxone-Associated Biliary Pseuodolithiasis: Sonographic and CT Findings
- Clinical Review and Case Report of Ceftriaxone-associated Gallbladder Pseudolithiasis in Adult
- Sonographic Findings of Ceftriaxone-associated Gallbladder Pseudolithiasis
- A Case of Reversible Biliary Pseudolithiasis After Ceftriaxone Therapy
- Biliary Pseudolithiasis in Children: To Avoid Unnecessary Surgical Procedure