J Korean Soc Radiol.
2011 Jun;64(6):603-609. 10.3348/jksr.2011.64.6.603.
Can We Predict Phyllodes Tumor among Fibroepithelial Lesions with Cellular Stroma Diagnosed at Breast Core Needle Biopsy?
- Affiliations
-
- 1Department of Radiology, CHA University College of Medicine, Korea.
- 2Department of Radiology, Yonsei University College of Medicine, Korea. ekkim@yuhs.ac
- KMID: 1443512
- DOI: http://doi.org/10.3348/jksr.2011.64.6.603
Abstract
- PURPOSE
To evaluate the surgical outcomes of fibroepithelial lesion with cellular stroma (FELCS) diagnosed at sonography guided core needle biopsy of breast masses, and to determine whether the clinical and imaging features of this lesion could predict the presence of a phyllodes tumor.
MATERIALS AND METHODS
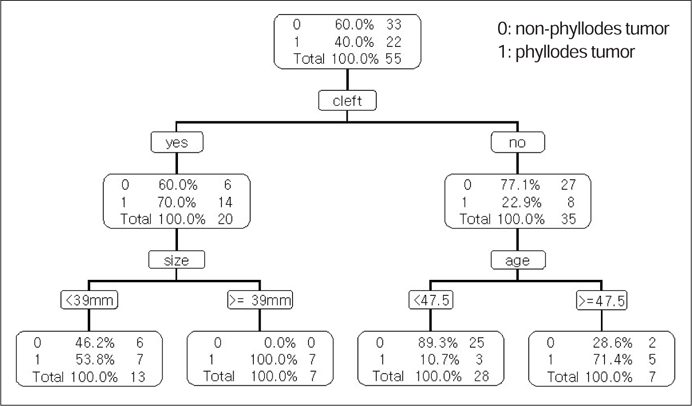
We retrospectively reviewed the pathologic results of sonography guided core needle biopsy of solid breast masses. A total of 55 FELCS diagnosed with this procedure that underwent subsequent surgical excision were included in this study; their medical records and radiologic images were retrospectively reviewed.
RESULTS
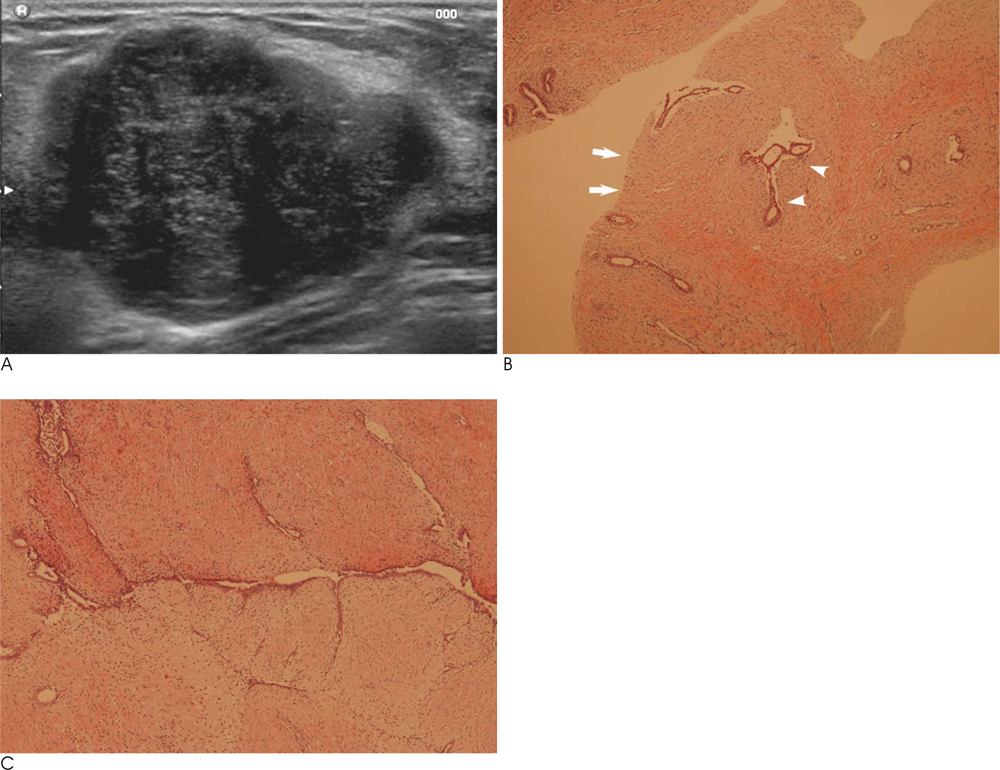
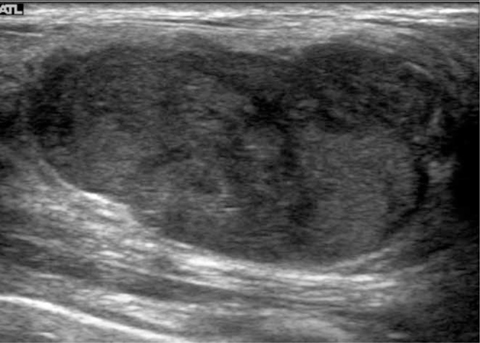
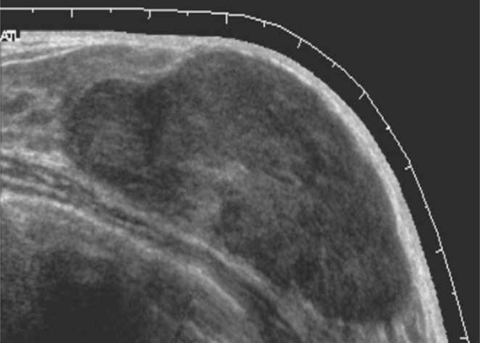
The results of the surgical excision revealed 22 (40%) phyllodes tumors and 33 (60%) non-phyllodes tumors: 30 (54.6%) fibroadenomas, 1 (1.8%) adenosis, 1 (1.8%) fibrocystic changes and 1 (1.8%) fibroadenomatous hyperplasia. Lesion size and patient age were significantly different between phyllodes tumors and non-phyllodes tumors groups (32.2 +/- 14.07 mm/22.4 +/- 13.64 mm, p=0.0078, 43.5 +/- 11.60 years/36.5 +/- 10.25 years, p=0.0207). Among the sonographic features, only cleft was significantly more visible in phyllodes tumors than in non-phyllodes tumors (n=14 (70%)/n=6 (30%), p=0.0016).
CONCLUSION
The size of the lesions, the age of the patients, and the sonographic features of cleft were the significant helpful variables to predict phyllodes tumors among FELCS diagnosed at breast core biopsy.
MeSH Terms
Figure
Reference
-
1. Jacobs TW, Chen YY, Guinee DG, Holden JA, Cha I, Bauermeister DE, et al. Fibroepithelial lesions with cellular stroma on breast core needle biopsy: are there predictors of outcome on surgical excision? . 2005; 124:342–354.2. Rosen PP. Fibroepithelial lesions. Rosen's breast pathology. 2nd ed. Philadelphia: Lipincott Williams & Williams;2001. p. 163–200.3. Shousha S. Issues in the interpretation of breast core biopsies. Int J Surg Pathol. 2003; 11:167–176.4. Bode MK, Rissanen T, Apaja-Sarkkinen M. Ultrasonography and core needle biopsy in the differential diagnosis of fibroadenoma and tumor phyllodes. Acta Radiol. 2007; 48:708–713.5. Jacobs TW, Connolly JL, Schnitt SJ. Nonmalignant lesions in breast core needle biopsies to excise or not to excise? Am J Surg Pathol. 2002; 26:1095–1110.6. Dershaw DD, Morris Ea, Liberman L, Abramson AF. Nondiagnostic stereotaxic core breast biopsy: results of rebiopsy. Radiology. 1996; 198:323–325.7. Meyer JE, Smith DN, Lester SC, DiPiro PJ, Denison CM, Harvey SC, et al. Large-needle core biopsy: nonmalignant breast abnormalities evaluated with surgical excision or repeat core biopsy. Radiology. 1998; 206:717–720.8. Komenaka IK, EL-Tammer M, Pile-Spellman E, Hibshoosh H. Core needle biopsy as a diagnostic tool to differentiate phyllodes tumor from fibroadenoma. Arch Surg. 2003; 138:987–990.9. Jung HK, Kim EK, Go KH, Rho JY. Phyllodes tumors or fibroepithelial lesions with cellular stroma of breast diagnosed at sonographically guided core needle biopsy: comparison between results on excision biopsy and sonographic findings. J Korean Soc Ultrasound Med. 2011; 30:45–53.10. Stravros AT. Atypical, high-risk, premalignant, and locally aggressive lesions. In : Stavros AT, editor. Breast Utrasound. Philadelphia: Lippincott, Williams & Wilkins;2001. p. 695–701.11. Reinfuss M, Mitus J, Duda K, Stelmach A, Rys J, Smolak K. The treatment and prognosis of patients with phyllodes tumor of the breast: an analysis of 170 cases. Cancer. 1996; 77:910–916.12. Salvadori B, Cusumano F, Del Bo R, Delledonne V, Grassi M, Rovini D, et al. Surgical treatment of phyllodes tumors of the breast. Cancer. 1989; 63:2532–2536.13. Jacklin RK, Ridgway PF, Ziprin P, Healy V, Hadjiminas D, Darzi A. Optimising preoperative diagnosis in phyllodes tumour of the breast. J Clin Pathol. 2006; 59:454–459.14. Chao Tc, Lo YF, Chen SC, Chen MF. Sonographic features of phyllodes tumors of the berast. Ultrasound Obstet Gynecol. 2002; 20:64–71.15. American College of Radiology. Breast imaging reporting and data system (BI-RADS). 4th ed. Reston, VA: American College of Radiology;2003.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Phyllodes Tumors and Fibroepithelial Lesions with Cellular Stroma of the Breast and Diagnosed by Sonographically Guided Core Needle Biopsy: A Comparison Between the Results of Excision Biopsy and the Sonographic Findings
- Benign core biopsy of probably benign breast lesions 2 cm or larger: correlation with excisional biopsy and long-term follow-up
- Breast Lesions with Discordant Results on Ultrasound-guided Core Needle Biopsy
- Recurrent Malignant Phyllodes Tumor with Liposarcoma
- Sonographic Features of Phyllodes Tumors of the Breast: A Pictorial Review