J Korean Soc Radiol.
2011 Jun;64(6):541-551. 10.3348/jksr.2011.64.6.541.
Evaluation of Agreement between 64-slice Computed Tomography Angiography and 201-Tl Single Photon Emission Computed Tomography-myocardial Perfusion Imaging in the Diagnosis of Significant Coronary Artery Disease
- Affiliations
-
- 1Department of Radiology, Ajou University School of Medicine, Korea. kdklsm@ajou.ac.kr
- 2Department of Nuclear Medicine, Ajou University School of Medicine, Korea.
- 3Department of Cardiology, Ajou University School of Medicine, Korea.
- KMID: 1443503
- DOI: http://doi.org/10.3348/jksr.2011.64.6.541
Abstract
- PURPOSE
To compare coronary computed tomography angiography (CTA) with single photon emission computed tomography-myocardial perfusion imaging (SPECT-MPI) for the detection of physiologically significant coronary artery disease (CAD).
MATERIALS AND METHODS
We evaluated 202 patients undergoing 64-slice coronary CTA and 201-Tl SPECT-MPI within a 3-month time interval. In addition, 68 patients underwent invasive coronary angiography (ICA). Coronary artery stenoses with luminal narrowing > or =50% were defined as "significant" on CTA and ICA. All myocardial segments were classified as reversible or fixed perfusion defects and normal segments on 201-Tl SPECT-MPI, and were allocated to the corresponding coronary vessels. Agreement and diagnostic performance between each imaging modality for physiologically significant CAD was calculated using the kappa (kappa) statistic and receiver operating characteristic analysis, respectively.
RESULTS
The sensitivity and specificity of CTA for the detection of physiologically significant CAD were 88% and 86% by patient-based analysis, and 84% and 91% by vessel-based analysis as compared to 201-Tl SPECT-MPI, respectively. The agreement between CTA and SPECTMPI was good (kappa = 0.647) and moderate (kappa = 0.558) by patient- and vessel-based analyses, respectively. The accuracy of CTA for predicting perfusion defects on SPECT-MPI was comparable (area under the curve; 0.814 vs. 0.819, p=0.902 on patient-based analysis, and 0.808 vs. 0.749, p=0.197 on vessel-based analysis) to ICA.
CONCLUSION
Coronary stenosis > or =50% on coronary CTA shows good agreement with perfusion defects in SPECT-MPI.
MeSH Terms
Figure
Reference
-
1. Klocke FJ, Baird MG, Lorell BH, Bateman TM, Messer JV, Berman DS, et al. ACC/AHA/ASNC guidelines for the clinical use of cardiac radionuclide imaging: executive summary - a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (ACC/AHA/ASNC Committee to Revise the 1995 Guidelines for the Clinical Use of Cardiac Radionuclide Imaging). J Am Coll Cardiol. 2003; 42:1318–1333.2. Topol EJ, Nissen SE. Our preoccupation with coronary luminology. The dissociation between clinical and angiographic findings in ischemic heart disease. Circulation. 1995; 92:2333–2242.3. White CW, Wright CB, Doty DB, Hiratza LF, Eastham CL, Harrison DG, et al. Does visual interpretation of the coronary arteriogram predict the physiologic importance of a coronary stenosis? N Engl J Med. 1984; 310:819–824.4. Leber AW, Knez A, von Ziegler F, Becker A, NikolaouK , Paul S, et al. Quantification of obstructive and nonobstructive coronary lesions by 64-slice computed tomography: a comparative study with quantitative coronary angiography and intravascular ultrasound. J Am Coll Cardiol. 2005; 46:147–154.5. Ropers D, Rixe J, Anders K, K¨ttener A, Baum U, Bautz W, et al. Usefulness of multidetector row spiral computed tomography with 64- × 0.6-mm collimation and 330-ms rotation for the noninvasive detection of significant coronary artery stenoses. Am J Cardiol. 2006; 97:343–348.6. Leber AW, Knez A, Becker A, Becker C, Ziegler F, Nikolaou K, et al. Accuracy of multidetector spiral computed tomography in identifying and differentiating the composition of coronary atherosclerotic plaques: a comparative study with intracoronary ultrasound. J Am Coll Cardiol. 2004; 43:1241–1247.7. Schuijf JD, Wijns W, Jukema JW, Atsma DE, Roos A, Lamb HJ, et al. Relationship between noninvasive coronary angiography with multi-slice computed tomography and myocardial perfusion imaging. J Am Coll Cardiol. 2006; 48:2508–2514.8. Hacker M, Jakobs T, Hack N, Nikolaou K, Becker C, Ziegler F, et al. Sixty-four slice spiral CT angiography does not predict the functional relevance of coronary artery stenoses in patients with stable angina. Eur J Nucl Med Mol Imaging. 2007; 34:4–10.9. Gaemperli O, Schepis T, Valenta I, Koepfli P, Husmann L, Scheffel H, Kaufmann PA, et al. Functionally relevant coronary artery disease: comparison of 64-section CT angiography with myocardial perfusion SPECT. Radiology. 2008; 248:414–423.10. Morise A, Evans M, Jalisi F, Shetty R, Stauffer M. A pretest prognostic score to assess patients undergoing exercise or pharmacological stress testing. Heart. 2007; 93:200–204.11. McCollough CH. Patient dose in cardiac computed tomography. Herz. 2003; 28:1–6.12. Dewey M, Rutsch W, Schnapauff D, Teige F, Hamm B. Coronary artery stenosis quantification using multislice computed tomography. Invest Radiol. 2007; 42:78–84.13. Cordeiro MA, Lardo AC, Brito MS, Neto MA, Siqueira MH, Parga JR, et al. CT angiography in highly calcified arteries: 2D manual vs. modified automated 3D approach to identify coronary stenoses. Int J Cardiovasc Imaging. 2006; 22:507–516.14. Leber AW, Johnson T, Becker A, Ziegler F, Tittus J, Nikolaou K, et al. Diagnostic accuracy of dual-source multi-slice CT-coronary angiography in patients with an intermediate pretest likelihood for coronary artery disease. Eur Heart J. 2007; 28:2354–2360.15. Cerqueira MD, Weissman NJ, Dilsizian V, Jacobs AK, Kaul S, Laskey WK, et al. Standardized myocardial segmentation and nomenclature for tomographic imaging of the heart: a statement for healthcare professionals from the Cardiac Imaging Committee of the Council on Clinical Cardiology of the American Heart Association. Circulation. 2002; 105:539–542.16. Austen WG, Edwards JE, Frye RL, Gensini GG, Gott VL, Griffith LS, et al. A reporting system on patients evaluated for coronary artery disease. Report of the Ad Hoc Committee for Grading of Coronary Artery Disease, Council on Cardiovascular Surgery, American Heart Association. Circulation. 1975; 51:5–40.17. Meng L, Cui L, Cheng Y, Wu X, Tang Y, Wang Y, et al. Effect of heart rate and coronary calcification on the diagnostic accuracy of the dual-source CT coronary angiography in patients with suspected coronary artery disease. Korean J Radiol. 2009; 10:347–354.18. Altman DG, Bland JM. Diagnostic tests 2: predictive values. BMJ. 1994; 309:102.19. Tamarappoo BK, Gutstein A, Cheng VY, Nakazato R, Gransar H, Dey D, et al. Assessment of the relationship between stenosis severity and distribution of coronary artery stenoses on multislice computed tomographic angiography and myocardial ischemia detected by single photon emission computed tomography. J Nucl Cardiol. 2010; 17:791–802.20. Gaemperli O, Schepis T, Koepfli P, Valenta I, Soyka J, Leschka S, et al. Accuracy of 64-slice CT angiography for the detection of functionally relevant coronary stenoses as assessed with myocardial perfusion SPECT. Eur J Nucl Med Mol Imaging. 2007; 34:1162–1171.21. Nicol ED, Schultz C, Stirrup J, Roughton M, Padley SP, Rubens MB, et al. Defining the appropriate CTA stenosis threshold for gatekeeping to invasive angiography: 50% or 70%? Int J Cardiol. 2010; 144:297–298.22. Gaemperli O, Husmann L, Schepis T, Koepfli P, Valenta I, Jenni W, et al. Coronary CT angiography and myocardial perfusion imaging to detect flow-limiting stenoses: a potential gatekeeper for coronary revascularization? Eur Heart J. 2009; 30:2921–2929.23. Rocha-Filho JA, Blankstein R, Shturman LD, Bezerra HG, Okada DR, Rogers IS, et al. Incremental value of adenosine-induced stress myocardial perfusion imaging with dual-source CT at cardiac CT angiography. Radiology. 2010; 254:410–419.24. Hacker M, Jakobs T, Matthiesen F, Nikolaou K, Becker C, Knez A, et al. Combined functional and morphological imaging consisting of gated myocardial perfusion SPECT and 16-detector multislice spiral CT angiography in the noninvasive evaluation of coronary artery disease: first experiences. Clin Imaging. 2007; 31:313–320.25. Hausleiter J, Meyer T, Hadamitzky M, Kastrati A, Martinoff S, Schomig A. Prevalence of noncalcified coronary plaques by 64-slice computed tomography in patients with an intermediate risk for significant coronary artery disease. J Am Coll Cardiol. 2006; 48:312–318.26. Chung SY, Lee KY, Chun EJ, Lee WW, Park EK, Chang HJ, et al. Comparison of stress perfusion MRI and SPECT for detection of myocardial ischemia in patients with angiographically proven three-vessel coronary artery disease. AJR Am J Roentgenol. 2010; 195:356–362.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Accuracy of Ventricular Volume and Ejection Fraction Measured by Gated Tl-201 Perfusion Single Photon Emission Tomography
- Myocardial SPECT
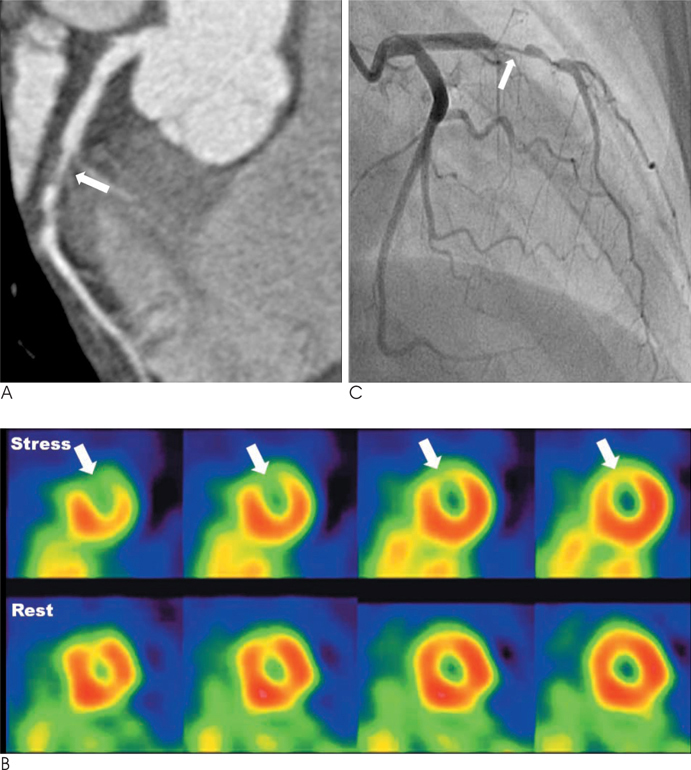
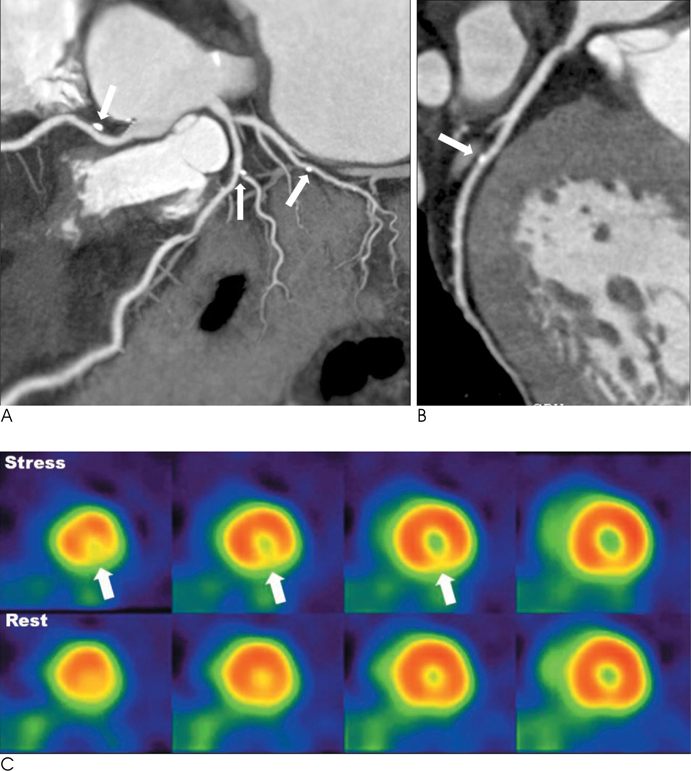
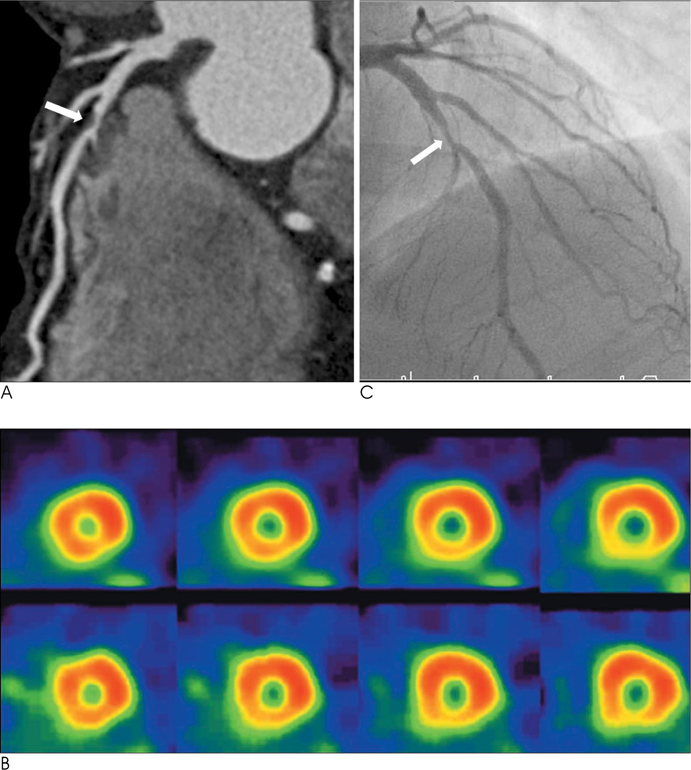
- Correlation Between Functional Myocardial Perfusion Imaging and Anatomical Cardiac CT in a Case of Myocardial Bridging
- Diagnosis of Coronary Artery Disease Using Myocardial Perfusion SPECT
- Prognostic Value of Rest Tl-201/Dipyridamole Stress Tc-99m-MIBI Myocardial Single Photon Emission Computed Tomography (SPECT)