J Korean Soc Radiol.
2011 Jul;65(1):89-93. 10.3348/jksr.2011.65.1.89.
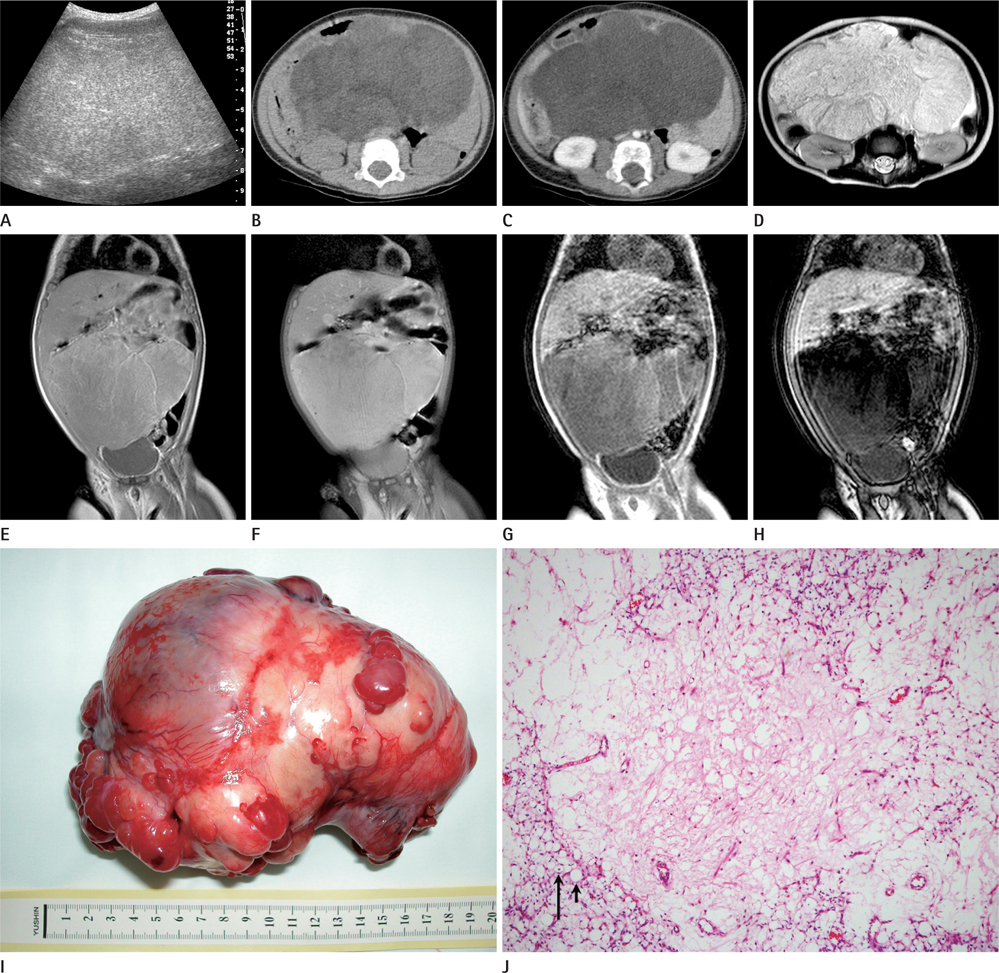
Identification of Fat in Myxoid Matrix-Rich Mesenteric Lipoblastoma Using In-Phase and Opposed-Phase MRI: A Case Report
- Affiliations
-
- 1Department of Radiology, Beijing Children's Hospital Affiliated to Capital Medical University, Beijing, China.
- 2Department of Radiology and Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. hwgoo@amc.seoul.kr
- KMID: 1443499
- DOI: http://doi.org/10.3348/jksr.2011.65.1.89
Abstract
- We present a rare case of a myxoid matrix-rich mesenteric lipoblastoma. In this case, fat-saturated T1-weighted magnetic resonance (MR) imaging failed to disclose the fatty component of the tumor, while in-phase and opposed-phase MR imaging could accurately identify small fat scattered in this myxoid matrix-rich tumor.
MeSH Terms
Figure
Reference
-
1. Bancroft LW, Kransdorf MJ, Peterson JJ, O'Connor MI. Benign fatty tumors: classification, clinical course, imaging appearance, and treatment. Skeletal Radiol. 2006; 35:719–733.2. Moholkar S, Sebire NJ, Roebuck DJ. Radiological-pathological correlation in lipoblastoma and lipoblastomatosis. Pediatr Radiol. 2006; 36:851–856.3. Mo YH, Peng SS, Li YW, Shun CT. Mesenteric lipoblastoma: case report. Pediatr Radiol. 2003; 33:37–40.4. Cudnik R, Efron PA, Chen MK, Reith JD, Beierle EA. Mesenteric lipoblastoma: a rare location in children. J Pediatr Surg. 2008; 43:e5–e7.5. Kelekis NL, Alexopoulou E, Brountzos EN, Ladis V, Boussiotou A, Kelekis DA. Giant adrenal myelolipoma with minimal fat content in a patient with homozygous beta-thalassemia: appearance on MRI. J Magn Reson Imaging. 2003; 18:608–611.6. Takahashi K, Inaoka T, Murakami N, Hirota H, Iwata K, Nagasawa K, et al. Characterization of the normal and hyperplastic thymus on chemical-shift MR imaging. AJR Am J Roentgenol. 2003; 180:1265–1269.7. Delfaut EM, Beltran J, Johnson G, Rousseau J, Marchandise X, Cotten A. Fat suppression in MR imaging: techniques and pitfalls. Radiographics. 1999; 19:373–382.8. Merkle EM, Nelson RC. Dual gradient-echo in-phase and opposed-phase hepatic MR imaging: a useful tool for evaluating more than fatty infiltration or fatty sparing. Radiographics. 2006; 26:1409–1418.9. Wang SF, Chang CY, Wu HD. Lipoblastomatosis of the shoulder: unusual MR appearance. Br J Radiol. 1998; 71:884–885.