J Korean Orthop Assoc.
2012 Feb;47(1):48-53. 10.4055/jkoa.2012.47.1.48.
Anatomical Study of the Pronator Quadratus Muscle and Comparison to Fracture Sites of the Distal Radius
- Affiliations
-
- 1Department of Orthopedic Surgery, Kosin University Gospel Hospital, Busan, Korea. jyujin2001@kosin.ac.kr
- 2Department of Orthopedic Surgery, Keimyung University School of Medicine, Daegu, Korea.
- KMID: 1439992
- DOI: http://doi.org/10.4055/jkoa.2012.47.1.48
Abstract
- PURPOSE
To collect data regarding the pronator-sparing approach using an anatomical study, which compared the fractures of the distal radius and pronator quadratus (PQ) muscle of an adult cadaveric radius.
MATERIALS AND METHODS
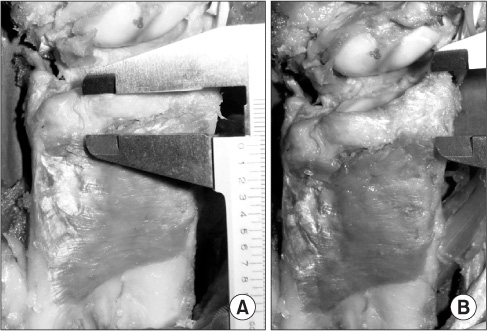
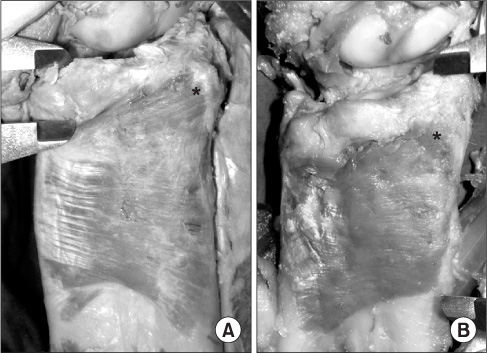
Fourteen adult cadaver wrists that did not have previous fractures or previous surgery and computed tomography data 32 fractures of the distal radius, were obtained. The size of the distal fracture fragment was measured using the picture archiving and communication system. The distance between the distal margin of the PQ muscles and the articular margin was measured using a caliper.
RESULTS
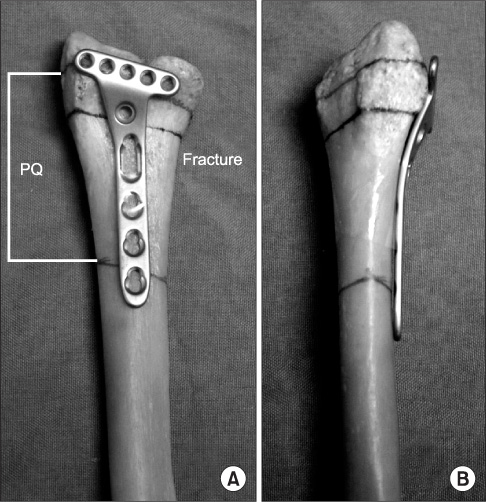
The PQ muscles had an average distance of 10.9 mm (range, 8-13 mm) from the radial styloid process and 10 mm (range, 8-12 mm) from the distal radioulnar joint (DRUJ). The fracture sites were located an average of 21.8 mm (range, 10-39 mm) from the radial styloid process and an average of 14.4 mm (range, 10-28 mm) from the DRUJ. Distal radial fractures overlapped an average of 11.8 mm from the radial styloid process and an average of 3.5 mm from the DRUJ.
CONCLUSION
The pronator-sparing approach could be applied to a functionally reduced fracture because the non-overlapping area of the distal fracture fragment was > or =10 mm and it is possible to repair the anatomic plate without detaching the PQ muscle.
Figure
Reference
-
1. Ring D. Nonunion of the distal radius. Hand Clin. 2005. 21:443–447.
Article2. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002. 27:205–215.
Article3. Byun YS. Minimally invasive plate osteosynthesis, MIPO. J Korean Fract Soc. 2007. 20:99–114.
Article4. Duncan SF, Weiland AJ. Minimally invasive reduction and osteosynthesis of articular fractures of the distal radius. Injury. 2001. 32:Suppl 1. SA14–SA24.
Article5. Imatani J, Noda T, Morito Y, Sato T, Hashizume H, Inoue H. Minimally invasive plate osteosynthesis for comminuted fractures of the metaphysis of the radius. J Hand Surg Br. 2005. 30:220–225.
Article6. Sen MK, Strauss N, Harvey EJ. Minimally invasive plate osteosynthesis of distal radius fractures using a pronator sparing approach. Tech Hand Up Extrem Surg. 2008. 12:2–6.
Article7. Downing ND, Karantana A. A revolution in the management of fractures of the distal radius? J Bone Joint Surg Br. 2008. 90:1271–1275.
Article8. Lee JC, Lim J, Chacha PB. The anatomical basis of the vascularized pronator quadratus pedicled bone graft. J Hand Surg Br. 1997. 22:644–646.
Article9. Rath S, Hung LK, Leung PC. Vascular anatomy of the pronator quadratus muscle-bone flap: a justification for its use with a distally based blood supply. J Hand Surg Am. 1990. 15:630–636.
Article10. Stuart PR. Pronator quadratus revisited. J Hand Surg Br. 1996. 21:714–722.
Article11. Gerber A, Masquelet AC. Anatomy and intracompartmental pressure measurement technique of the pronator quadratus compartment. J Hand Surg Am. 2001. 26:1129–1134.
Article12. Kupfer D, Lister G. The pronator quadratus muscle flap: coverage of the osteotomized radius following elevation of the radial forearm flap. Plast Reconstr Surg. 1992. 90:1093–1095.13. Svízenská I, Cizmár I, Visna P. An anatomical study of the anterior interosseous nerve and its innervation of the pronator quadratus muscle. J Hand Surg Br. 2005. 30:635–637.14. Lamas C, Llusà M, Méndez A, Proubasta I, Carrera A, Forcada P. Intraosseous vascularity of the distal radius: anatomy and clinical implications in distal radius fractures. Hand (N Y). 2009. 4:418–423.
Article15. Ekenstam F. Osseous anatomy and articular relationships about the distal ulna. Hand Clin. 1998. 14:161–164.
Article16. Garcia-Elias M. Soft-tissue anatomy and relationships about the distal ulna. Hand Clin. 1998. 14:165–176.
Article17. Gordon KD, Dunning CE, Johnson JA, King GJ. Influence of the pronator quadratus and supinator muscle load on DRUJ stability. J Hand Surg Am. 2003. 28:943–950.
Article18. Orbay JL, Badia A, Indriago IR, et al. The extended flexor carpi radialis approach: a new perspective for the distal radius fracture. Tech Hand Up Extrem Surg. 2001. 5:204–211.
Article19. Koh S, Andersen CR, Buford WL Jr, Patterson RM, Viegas SF. Anatomy of the distal brachioradialis and its potential relationship to distal radius fracture. J Hand Surg Am. 2006. 31:2–8.
Article20. Agee JM. Distal radius fractures. Multiplanar ligamentotaxis. Hand Clin. 1993. 9:577–585.21. Fernández DL. Fractures of the distal radius: operative treatment. Instr Course Lect. 1993. 42:73–88.22. Krettek C, Schandelmaier P, Miclau T, Tscherne H. Minimally invasive percutaneous plate osteosynthesis (MIPPO) using the DCS in proximal and distal femoral fractures. Injury. 1997. 28:Suppl 1. A20–A30.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Fate of Pronator Quadratus Muscle after Volar Locking Plating of Unstable Distal Radius Fractures
- Ultrasonographic Assessment of the Pronator Quadratus Muscle after Surgical Treatment for Distal Radius Fractures
- Examination of the Pronator Quadratus Muscle during Hardware Removal Procedures after Volar Plating for Distal Radius Fractures
- Treatment of Scaphoid Nonunions Using a Pronator Quadratus Pedicled Bone Graft
- Comparison of Distal Radius Fractures with or without Scaphoid Fractures