J Korean Bone Joint Tumor Soc.
2012 Dec;18(2):83-88. 10.5292/jkbjts.2012.18.2.83.
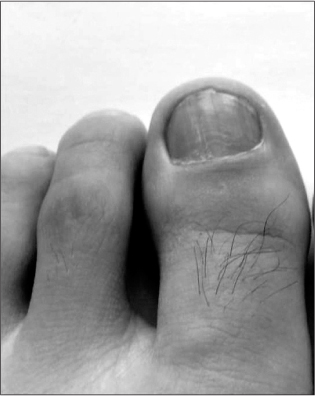
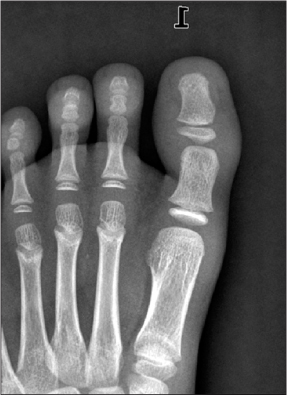
Thin Split-Thickness Toe Nail-Bed Grafts for Nail Bed Defects in Subungal Exostosis: Two Cases Report
- Affiliations
-
- 1Department of Orthopaedic Surgery, Dongguk University College of Medicine, Seongnam, Korea. drlsh@hanmail.net
- 2Department of Pathology, Dongguk University College of Medicine, Seongnam, Korea.
- 3Department of Orthopedic Surgery, Armed Forces Capital Hospital, Seongnam, Korea.
- KMID: 1431675
- DOI: http://doi.org/10.5292/jkbjts.2012.18.2.83
Abstract
- We reviewed the clinical features of 2 patients who underwent surgery for subungal exostosis, focusing on postoperative deformity of the nail. The lesion destroyed the nail bed and was excised with a direct approach. then thin split-thickness sterile matrix graft was done after excision of the tumor because the defect of the nail bed was large. Good postoperative appearance of the nail was obtained by thin split-thickness sterile matrix graft. The use of thin split-thickness sterile matrix graft for the replacement of a nail bed defect can regain a smooth, adherent, and normal-looking nail and avoid donor-site morbidity. Thin split-thickness toe-nail bed graft is a good choice for the prevention of postoperative deformity.
Figure
Reference
-
1. Hatoko M, Tanaka A, Kuwahara M, et al. Hard palate mucosal grafts for defects of the nail bed. Ann Plast Surg. 2002. 49:424–428.2. Dumontier CA, Abimelec P. Nail unit enchondromas and osteochondromas: a surgical approach. Dermatol Surg. 2001. 27:274–279.3. Lokiec F, Ezra E, Krasin E, Keret D, Wientroub S. A simple and efficient surgical technique for subungual exostosis. J Pediatr Orthop. 2001. 21:76–79.4. Iizuka T, Kinoshita Y, Fukumoto K. Subungual exostosis of the finger. Ann Plast Surg. 1995. 35:330–332.5. Ilyas W, Geskin L, Joseph AK, Seraly MP. Subungual exostosis of the third toe. J Am Acad Dermatol. 2001. 45:6 Suppl. S200–S201.6. Dahlin DC. Bone tumor: general aspects and data on 8542 cases. 1986. 4th ed. Springerfield, Illinois: Charles C Thomas;19–30.7. Landon GC, Johnson KA, Dahlin DC. Subungual exostoses. J Bone Joint Surg Am. 1979. 61:256–259.8. de Palma L, Gigante A, Specchia N. Subungual exostosis of the foot. Foot Ankle Int. 1996. 17:758–763.9. Moon MS, Lee IJ, Chung KH. Subungual exostoeis. J Korean Orthop Assoc. 1986. 21:502–506.10. Koshima I, Soeda S, Takase T, Yamasaki M. Free vascularized nail grafts. J Hand Surg Am. 1988. 13:29–32.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Tratment of the Nail Bed Avulsion Injury with Split-thickness Nail Bed Graft
- Subungal Exostosis
- Immediate Nail Bed Graft on Exposed Distal Phalanx in Fingertip Injury
- Simultaneous Volar Pulp and Nail Bed Reconstruction with the Second Toe Onychocutaneous Free Flap
- Nail bed defect reconstruction using a thenar fascial flap and subsequent nail bed grafting