Korean J Radiol.
2013 Feb;14(1):132-137. 10.3348/kjr.2013.14.1.132.
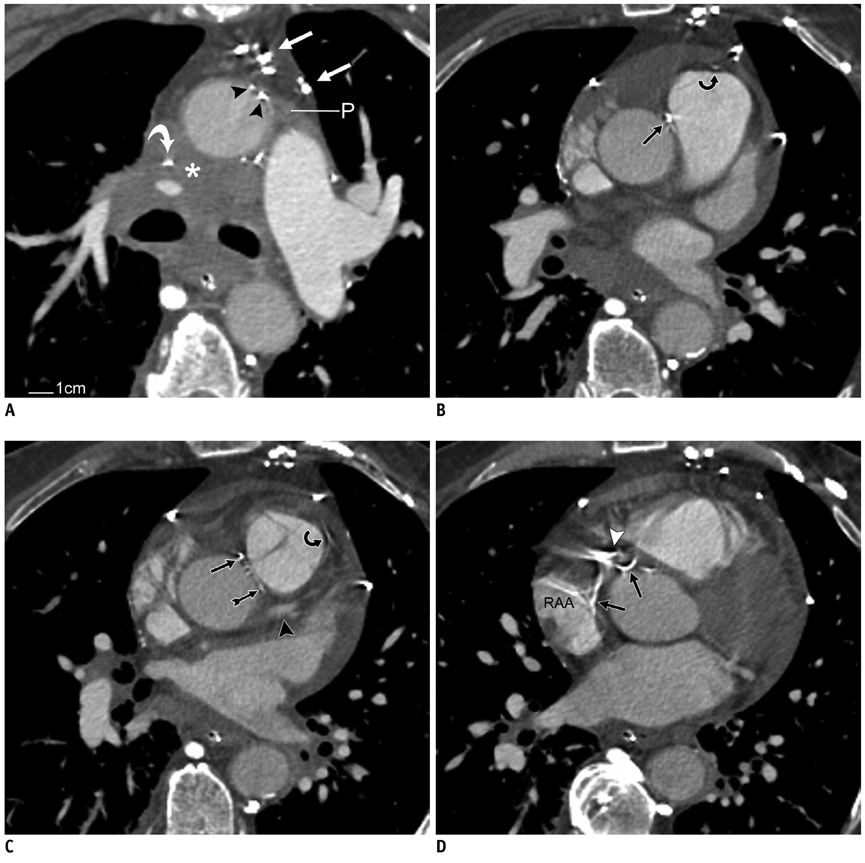
CT Demonstration of the Extracardiac Anastomoses of the Coronary Veins in Superior Vena Cava or Left Brachiocephalic Vein Obstruction
- Affiliations
-
- 1Department of Diagnostic Radiology, Montreal General Hospital, McGill University Health Centre, Montreal, Quebec H3G 1A4, Canada. joseph.casullo@muhc.mcgill.ca
- KMID: 1430057
- DOI: http://doi.org/10.3348/kjr.2013.14.1.132
Abstract
- CT scans in four cases of chronic superior vena cava or left brachiocephalic vein obstruction demonstrate a systemic-to-cardiac collateral venous pathway through anastomoses between the pericardial branches of systemic veins and the presumed adventitial veins of the ascending aorta and pulmonary trunk. These adventitial veins then drain into tributaries of the anterior cardiac veins or ventricular coronary veins.
Keyword
MeSH Terms
Figure
Reference
-
1. Cihangiroglu M, Lin BH, Dachman AH. Collateral pathways in superior vena caval obstruction as seen on CT. J Comput Assist Tomogr. 2001. 25:1–8.2. Kapur S, Paik E, Rezaei A, Vu DN. Where there is blood, there is a way: unusual collateral vessels in superior and inferior vena cava obstruction. Radiographics. 2010. 30:67–78.3. Haller A von. First lines of physiology. A reprint of the 1786 edition. Sources of science; series no. 32. 1966. New York: Johnson Reprint Corp;49.4. Baroldi G, Scomazzoni G. Coronary circulation in the normal and the pathologic heart. 1965. Washington, DC: Armed Forces Institute of Pathology;79.5. Clarke JA. An X-ray microscopic study of the vasa vasorum of the normal human ascending aorta. Br Heart J. 1965. 27:99–104.6. Clarke JA. An x-ray microscopic study of the vasa vasorum of the normal human pulmonary trunk. Acta Anat (Basel). 1965. 61:6–14.7. Schaffler GJ, Groell R, Peichel KH, Rienmüller R. Imaging the coronary venous drainage system using electron-beam CT. Surg Radiol Anat. 2000. 22:35–39.8. Ortale JR, Marquez CQ. Anatomy of the intramural venous sinuses of the right atrium and their tributaries. Surg Radiol Anat. 1998. 20:23–29.9. von Lüdinghausen M, Ohmachi N, Besch S, Mettenleiter A. Atrial veins of the human heart. Clin Anat. 1995. 8:169–189.10. Sugiyama H, Yoo SJ, Williams W, Benson LN. Characterization and treatment of systemic venous to pulmonary venous collaterals seen after the Fontan operation. Cardiol Young. 2003. 13:424–430.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Double Left Brachiocephalic Veins with Persistent Left Superior Vena Cava: A Case Report
- Circumaortic Left Brachiocephalic Vein: CT Findings
- A Case of Behcet's Disease with Superior Vena Cava Syndrome
- Bypass of Superior Vena Cava with Spiral Vein Graft
- A Case of the Malformation of Azygos and Hemiazygos System