J Korean Orthop Assoc.
2013 Apr;48(2):142-150. 10.4055/jkoa.2013.48.2.142.
Implant Selection for Treatment of Distal Radius Fractures
- Affiliations
-
- 1Department of Orthopedic Surgery, St. Vincent's Hospital, The Catholic University of Korea, Suwon, Korea. jylos1@gmail.com
- KMID: 1424107
- DOI: http://doi.org/10.4055/jkoa.2013.48.2.142
Abstract
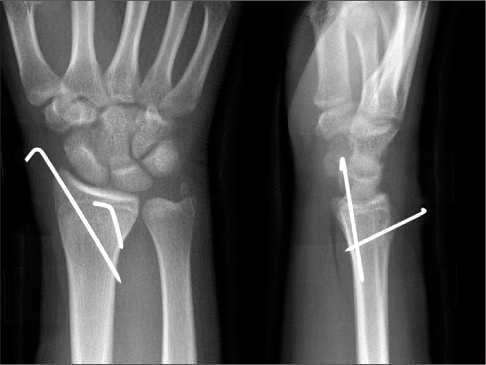
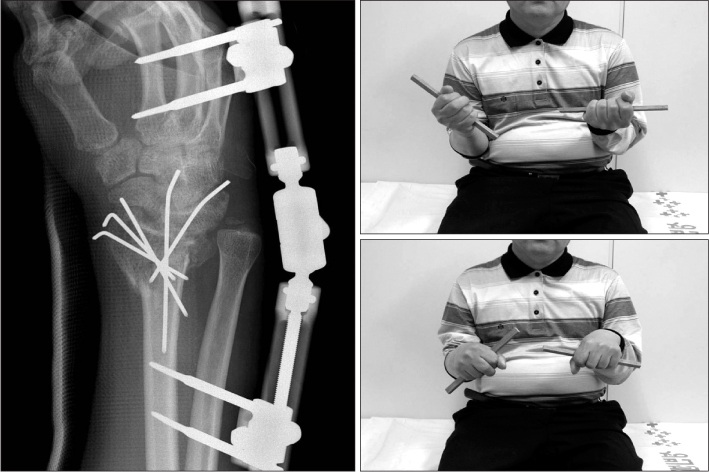
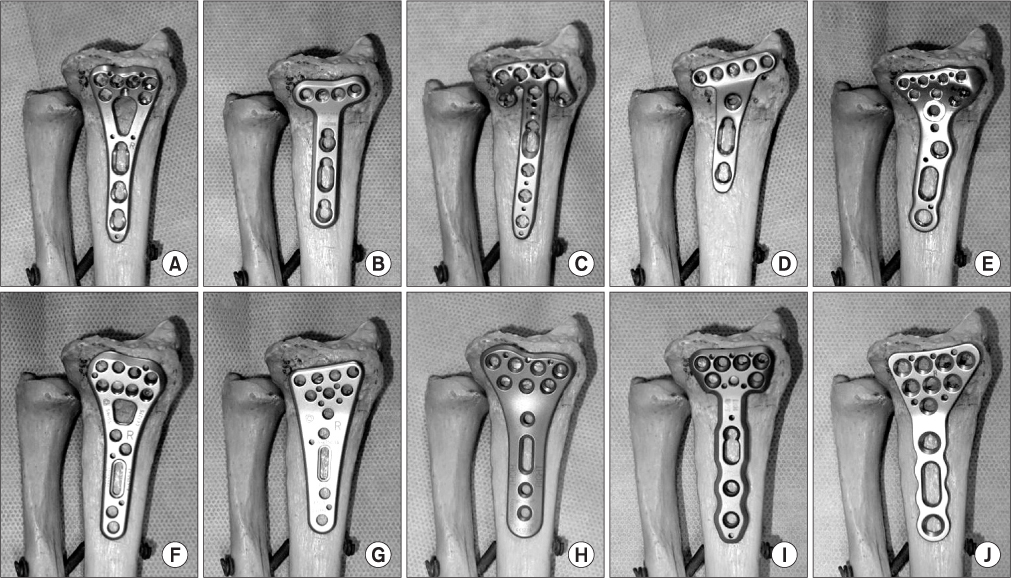
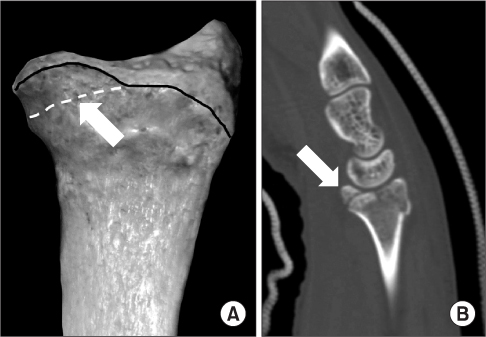
- Anatomical reduction is essential for successful treatment of distal radius fractures. In-depth understanding of the implant is mandatory in order to obtain adequate fixation of the fracture fragments and to avoid implant-related complications. Selection of an improper implant and screw length may lead to rupture of flexor or extensor tendon as a complication. This article will briefly discuss the pros and cons of the traditional fixation methods such as percutaneous pin fixation and external fixation, and will focus on the recent development of the volar locking plate. Variable-angle locking plate, which was introduced in an effort to provide surgeons with more freedom for fixation, may have inadequate fixation strength if screw locking is repeated. From the biomechanical study, at least four distal locking screws are enough to have strength to maintain fracture fixation. Measuring screw length may be difficult; therefore, information about the ratio of the metaphysis and diaphysis will be helpful in deciding on the proper screw length. Locking screws are recommended as they are stronger than locking pegs. In order to avoid flexor tendon ruptures, the plate should not be placed too far distally.
Figure
Reference
-
1. Chung KC, Spilson SV. The frequency and epidemiology of hand and forearm fractures in the United States. J Hand Surg Am. 2001. 26:908–915.
Article2. Park C, Ha YC, Jang S, Jang S, Yoon HK, Lee YK. The incidence and residual lifetime risk of osteoporosis-related fractures in Korea. J Bone Miner Metab. 2011. 29:744–751.
Article3. Clancey GJ. Percutaneous Kirschner-wire fixation of Colles fractures. A prospective study of thirty cases. J Bone Joint Surg Am. 1984. 66:1008–1014.
Article4. Habernek H, Weinstabl R, Fialka C, Schmid L. Unstable distal radius fractures treated by modified Kirschner wire pinning: anatomic considerations, technique, and results. J Trauma. 1994. 36:83–88.5. Munson GO, Gainor BJ. Percutaneous pinning of distal radius fractures. J Trauma. 1981. 21:1032–1035.
Article6. Kapandji A. Intra-focal pinning of fractures of the distal end of the radius 10 years later. Ann Chir Main. 1987. 6:57–63.7. Glickel SZ, Catalano LW, Raia FJ, Barron OA, Grabow R, Chia B. Long-term outcomes of closed reduction and percutaneous pinning for the treatment of distal radius fractures. J Hand Surg Am. 2008. 33:1700–1705.
Article8. Barton T, Chambers C, Lane E, Bannister G. Do Kirschner wires maintain reduction of displaced Colles' fractures? Injury. 2005. 36:1431–1434.
Article9. Anderson R, O'Neil G. Comminuted fractures of the distal end of the radius. Surg Gynecol Obstet. 1944. 78:434–440.10. Kreder HJ, Hanel DP, Agel J, et al. Indirect reduction and percutaneous fixation versus open reduction and internal fixation for displaced intra-articular fractures of the distal radius: a randomised, controlled trial. J Bone Joint Surg Br. 2005. 87:829–836.11. Bartosh RA, Saldana MJ. Intraarticular fractures of the distal radius: a cadaveric study to determine if ligamentotaxis restores radiopalmar tilt. J Hand Surg Am. 1990. 15:18–21.
Article12. Kaempffe FA, Walker KM. External fixation for distal radius fractures: effect of distraction on outcome. Clin Orthop Relat Res. 2000. 380:220–225.
Article13. Kaempffe FA, Wheeler DR, Peimer CA, Hvisdak KS, Ceravolo J, Senall J. Severe fractures of the distal radius: effect of amount and duration of external fixator distraction on outcome. J Hand Surg Am. 1993. 18:33–41.
Article14. Raju P, Kini SG. Loss of correction in unstable comminuted distal radius fractures with external fixation and bone grafting--a long term followup study. J Orthop Surg Res. 2011. 6:23.15. Axelrod TS, McMurtry RY. Open reduction and internal fixation of comminuted, intraarticular fractures of the distal radius. J Hand Surg Am. 1990. 15:1–11.
Article16. Bradway JK, Amadio PC, Cooney WP. Open reduction and internal fixation of displaced, comminuted intra-articular fractures of the distal end of the radius. J Bone Joint Surg Am. 1989. 71:839–847.
Article17. Jupiter JB, Lipton H. The operative treatment of intraarticular fractures of the distal radius. Clin Orthop Relat Res. 1993. 292:48–61.
Article18. Rikli DA, Regazzoni P. Fractures of the distal end of the radius treated by internal fixation and early function. A preliminary report of 20 cases. J Bone Joint Surg Br. 1996. 78:588–592.19. Yu YR, Makhni MC, Tabrizi S, Rozental TD, Mundanthanam G, Day CS. Complications of low-profile dorsal versus volar locking plates in the distal radius: a comparative study. J Hand Surg Am. 2011. 36:1135–1141.
Article20. Rausch S, Klos K, Stephan H, et al. Evaluation of a polyaxial angle-stable volar plate in a distal radius C-fracture model--a biomechanical study. Injury. 2011. 42:1248–1252.21. Stanbury SJ, Salo A, Elfar JC. Biomechanical analysis of a volar variable-angle locking plate: the effect of capturing a distal radial styloid fragment. J Hand Surg Am. 2012. 37:2488–2494.
Article22. Marlow WJ, Singhal R, Dheerendra S, Ralte P, Fischer J, Waseem M. Distal radius volar locking plates: does a variable angle locking system confer a clinical advantage? Acta Orthop Belg. 2012. 78:309–316.23. Orbay JL, Fernandez DL. Volar fixation for dorsally displaced fractures of the distal radius: a preliminary report. J Hand Surg Am. 2002. 27:205–215.
Article24. Drobetz H, Weninger P, Grant C, et al. More is not necessarily better. A biomechanical study on distal screw numbers in volar locking distal radius plates. Injury. 2013. 44:535–539.
Article25. Moss DP, Means KR Jr, Parks BG, Forthman CL. A biomechanical comparison of volar locked plating of intra-articular distal radius fractures: use of 4 versus 7 screws for distal fixation. J Hand Surg Am. 2011. 36:1907–1911.
Article26. Mehling I, Müller LP, Delinsky K, Mehler D, Burkhart KJ, Rommens PM. Number and locations of screw fixation for volar fixed-angle plating of distal radius fractures: biomechanical study. J Hand Surg Am. 2010. 35:885–891.
Article27. Neuhaus V, Badri O, Ferree S, Bot AG, Ring DC, Mudgal CS. Radiographic alignment of unstable distal radius fractures fixed with 1 or 2 rows of screws in volar locking plates. J Hand Surg Am. 2013. 38:297–301.
Article28. Wall LB, Brodt MD, Silva MJ, Boyer MI, Calfee RP. The effects of screw length on stability of simulated osteoporotic distal radius fractures fixed with volar locking plates. J Hand Surg Am. 2012. 37:446–453.
Article29. Park DH, Goldie BS. Volar plating for distal radius fractures--do not trust the image intensifier when judging distal subchondral screw length. Tech Hand Up Extrem Surg. 2012. 16:169–172.
Article30. Riddick AP, Hickey B, White SP. Accuracy of the skyline view for detecting dorsal cortical penetration during volar distal radius fixation. J Hand Surg Eur Vol. 2012. 37:407–411.
Article31. Weninger P, Dall'Ara E, Leixnering M, et al. Volar fixed-angle plating of extra-articular distal radius fractures--a biomechanical analysis comparing threaded screws and smooth pegs. J Trauma. 2010. 69:E46–E55.
Article32. Martineau PA, Waitayawinyu T, Malone KJ, Hanel DP, Trumble TE. Volar plating of AO C3 distal radius fractures: biomechanical evaluation of locking screw and locking smooth peg configurations. J Hand Surg Am. 2008. 33:827–834.
Article33. Harness NG, Jupiter JB, Orbay JL, Raskin KB, Fernandez DL. Loss of fixation of the volar lunate facet fragment in fractures of the distal part of the radius. J Bone Joint Surg Am. 2004. 86:1900–1908.
Article34. Soong M, van Leerdam R, Guitton TG, Got C, Katarincic J, Ring D. Fracture of the distal radius: risk factors for complications after locked volar plate fixation. J Hand Surg Am. 2011. 36:3–9.
Article35. Matityahu AM, Lapalme SN, Seth A, Marmor MT, Buckley JM, Lattanza LL. How placement affects force and contact pressure between a volar plate of the distal radius and the flexor pollicus longus tendon: a biomechanical investigation. J Hand Surg Eur Vol. 2013. 38:144–150.
Article36. Brown EN, Lifchez SD. Flexor pollicis longus tendon rupture after volar plating of a distal radius fracture: pronator quadratus plate coverage may not adequately protect tendons. Eplasty. 2011. 11:e43.37. Imatani J, Akita K, Yamaguchi K, Shimizu H, Kondou H, Ozaki T. An anatomical study of the watershed line on the volar, distal aspect of the radius: implications for plate placement and avoidance of tendon ruptures. J Hand Surg Am. 2012. 37:1550–1554.
Article38. Drobetz H, Bryant AL, Pokorny T, Spitaler R, Leixnering M, Jupiter JB. Volar fixed-angle plating of distal radius extension fractures: influence of plate position on secondary loss of reduction--a biomechanic study in a cadaveric model. J Hand Surg Am. 2006. 31:615–622.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Complications of Distal Radius Fracture
- Operative Treatment of Unstable Fracture of Distal Radius
- The Usefulness of Computed Tomography in Distal Radius Fractures Involving Articular Surface
- Arthroscopically Assisted Reduction of Distal Radius Fractures
- Surgical Treatment of Distal Radius Fractures and Treatment of Common Accompanying Lesions