Clin Orthop Surg.
2013 Mar;5(1):66-73. 10.4055/cios.2013.5.1.66.
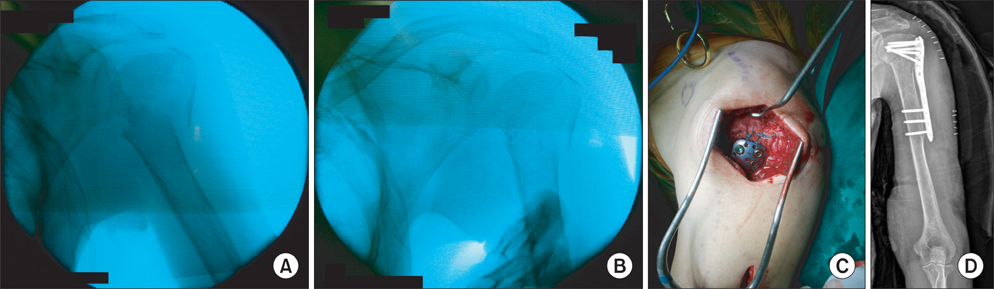
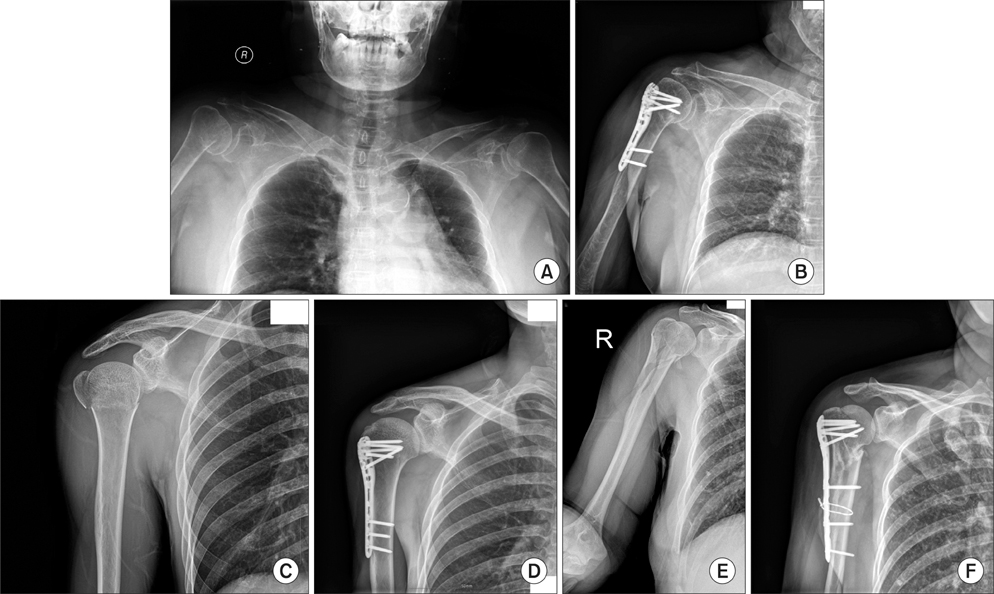
Indirect Reduction Maneuver and Minimally Invasive Approach for Displaced Proximal Humerus Fractures in Elderly Patients
- Affiliations
-
- 1Department of Orthopaedic Surgery, Samsung Changwon Hospital, Sungkyunkwan University School of Medicine, Changwon, Korea. can1204@hanmail.net
- KMID: 1402328
- DOI: http://doi.org/10.4055/cios.2013.5.1.66
Abstract
- BACKGROUND
This study examined the clinical outcomes of indirect reduction maneuver and minimally invasive approach for treating displaced proximal humerus fractures in patients older than 60.
METHODS
Thirty-two patients (11 male and 21 female) who had undergone treatment for displaced proximal humerus fracture were evaluated. The mean age of the patients was 72.4 years (range, 60 to 92 years). All cases were followed up for at least 12 months. All patients were interviewed and evaluated on the visual analog scale, with gender-specific constant score correction for age, standardized X-rays to check the neck-shaft angle (NSA) and the presence of medial support, and bone mineral density. Statistical analysis was performed with a multiple regression analysis.
RESULTS
The average visual analog scale score was 2.4, and the average gender-specific constant score correction for age was 80.6 points. Final functional outcomes were 8 excellent, 15 good, 7 fair, and 2 poor. The average NSA was 122.8degrees; and the radiological results were 20 good, 11 fair, and 1 poor. There was significant difference of the gender-specific constant score for age between the group of NSA more than 110degrees and the group of NSA less than 110degrees (p = 0.00). There were 26 cases with and 6 cases without medial support, with significant difference between the gender-specific constant score correction for age of these groups (p = 0.01). Complications occurred in 4 patients (12.5%).
CONCLUSIONS
The indirect reduction maneuver and minimally invasive approach were safe and reliable options for the treatment of displaced proximal humerus fractures in the elderly patients. An inadequate reduction (i.e., less than 110degrees NSA) or lack of medial support (e.g., no cortical or screw support) were significant factors contributing to poor functional outcomes.
MeSH Terms
Figure
Cited by 1 articles
-
Minimally Invasive Plate Osteosynthesis Using a Screw Compression Method for Treatment of Humeral Shaft Fractures
Sang-Hun Ko, Jae-Ryong Cha, Chae Chil Lee, Yong Tae Joo, Kyeong Su Eom
Clin Orthop Surg. 2017;9(4):506-513. doi: 10.4055/cios.2017.9.4.506.
Reference
-
1. Bogner R, Hubner C, Matis N, Auffarth A, Lederer S, Resch H. Minimally-invasive treatment of three- and four-part fractures of the proximal humerus in elderly patients. J Bone Joint Surg Br. 2008. 90(12):1602–1607.2. Krappinger D, Bizzotto N, Riedmann S, Kammerlander C, Hengg C, Kralinger FS. Predicting failure after surgical fixation of proximal humerus fractures. Injury. 2011. 42(11):1283–1288.3. Lau TW, Leung F, Chan CF, Chow SP. Minimally invasive plate osteosynthesis in the treatment of proximal humeral fracture. Int Orthop. 2007. 31(5):657–664.4. Kralinger F, Gschwentner M, Wambacher M, Smekal V, Haid C. Proximal humeral fractures: what is semi-rigid? Biomechanical properties of semi-rigid implants, a biomechanical cadaver based evaluation. Arch Orthop Trauma Surg. 2008. 128(2):205–210.5. Rancan M, Dietrich M, Lamdark T, Can U, Platz A. Minimal invasive long PHILOS®-plate osteosynthesis in metadiaphyseal fractures of the proximal humerus. Injury. 2010. 41(12):1277–1283.6. Neer CS 2nd. Displaced proximal humeral fractures. I Classification and evaluation. J Bone Joint Surg Am. 1970. 52(6):1077–1089.7. Marsh JL, Slongo TF, Agel J, et al. Fracture and dislocation classification compendium-2007: Orthopaedic Trauma Association classification, database and outcomes committee. J Orthop Trauma. 2007. 21:10 Suppl. S1–S133.8. Constant CR, Murley AH. A clinical method of functional assessment of the shoulder. Clin Orthop Relat Res. 1987. (214):160–164.9. Paavolainen P, Bjorkenheim JM, Slatis P, Paukku P. Operative treatment of severe proximal humeral fractures. Acta Orthop Scand. 1983. 54(3):374–379.10. Gardner MJ, Weil Y, Barker JU, Kelly BT, Helfet DL, Lorich DG. The importance of medial support in locked plating of proximal humerus fractures. J Orthop Trauma. 2007. 21(3):185–191.11. Gardner MJ, Griffith MH, Lorich DG. Helical plating of the proximal humerus. Injury. 2005. 36(10):1197–1200.12. Smith J, Berry G, Laflamme Y, Blain-Pare E, Reindl R, Harvey E. Percutaneous insertion of a proximal humeral locking plate: an anatomic study. Injury. 2007. 38(2):206–211.13. Thanasas C, Kontakis G, Angoules A, Limb D, Giannoudis P. Treatment of proximal humerus fractures with locking plates: a systematic review. J Shoulder Elbow Surg. 2009. 18(6):837–844.14. Sproul RC, Iyengar JJ, Devcic Z, Feeley BT. A systematic review of locking plate fixation of proximal humerus fractures. Injury. 2011. 42(4):408–413.15. Kobayashi M, Watanabe Y, Matsushita T. Early full range of shoulder and elbow motion is possible after minimally invasive plate osteosynthesis for humeral shaft fractures. J Orthop Trauma. 2010. 24(4):212–216.16. Roderer G, Erhardt J, Graf M, Kinzl L, Gebhard F. Clinical results for minimally invasive locked plating of proximal humerus fractures. J Orthop Trauma. 2010. 24(7):400–406.17. Lill H, Hepp P, Korner J, et al. Proximal humeral fractures: how stiff should an implant be? A comparative mechanical study with new implants in human specimens. Arch Orthop Trauma Surg. 2003. 123(2-3):74–81.18. Boileau P, Pennington SD, Alami G. Proximal humeral fractures in younger patients: fixation techniques and arthroplasty. J Shoulder Elbow Surg. 2011. 20:2 Suppl. S47–S60.19. Rouleau DM, Laflamme GY, Berry GK, Harvey EJ, Delisle J, Girard J. Proximal humerus fractures treated by percutaneous locking plate internal fixation. Orthop Traumatol Surg Res. 2009. 95(1):56–62.20. Resch H, Hubner C, Schwaiger R. Minimally invasive reduction and osteosynthesis of articular fractures of the humeral head. Injury. 2001. 32:Suppl 1. SA25–SA32.21. Solberg BD, Moon CN, Franco DP, Paiement GD. Surgical treatment of three and four-part proximal humeral fractures. J Bone Joint Surg Am. 2009. 91(7):1689–1697.22. Liu KY, Chen TH, Shyu JF, Wang ST, Liu JY, Chou PH. Anatomic study of the axillary nerve in a Chinese cadaveric population: correlation of the course of the nerve with proximal humeral fixation with intramedullary nail or external skeletal fixation. Arch Orthop Trauma Surg. 2011. 131(5):669–674.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- An Anterosuperior Deltoid Splitting Approach for Plate Fixation of Proximal Humeral Fractures
- Percutaneous Pinning & External Fixation In the Treatment of Proximal Humerus Fracture
- Minimally Invasive Anterior Approach in Open Reduction of Displaced Supracondylar Fractures of Humerus in Children
- Closed Reduction and Percutaneous Fixation in the Treatment of Proximal Humerus Fractures
- Minimally Invasive Plate Osteosynthesis for Humeral Proximal or Distal Shaft Fractures Using a 3.5/5.0 Metaphyseal Locking Plate