J Korean Med Sci.
2007 Aug;22(4):740-745. 10.3346/jkms.2007.22.4.740.
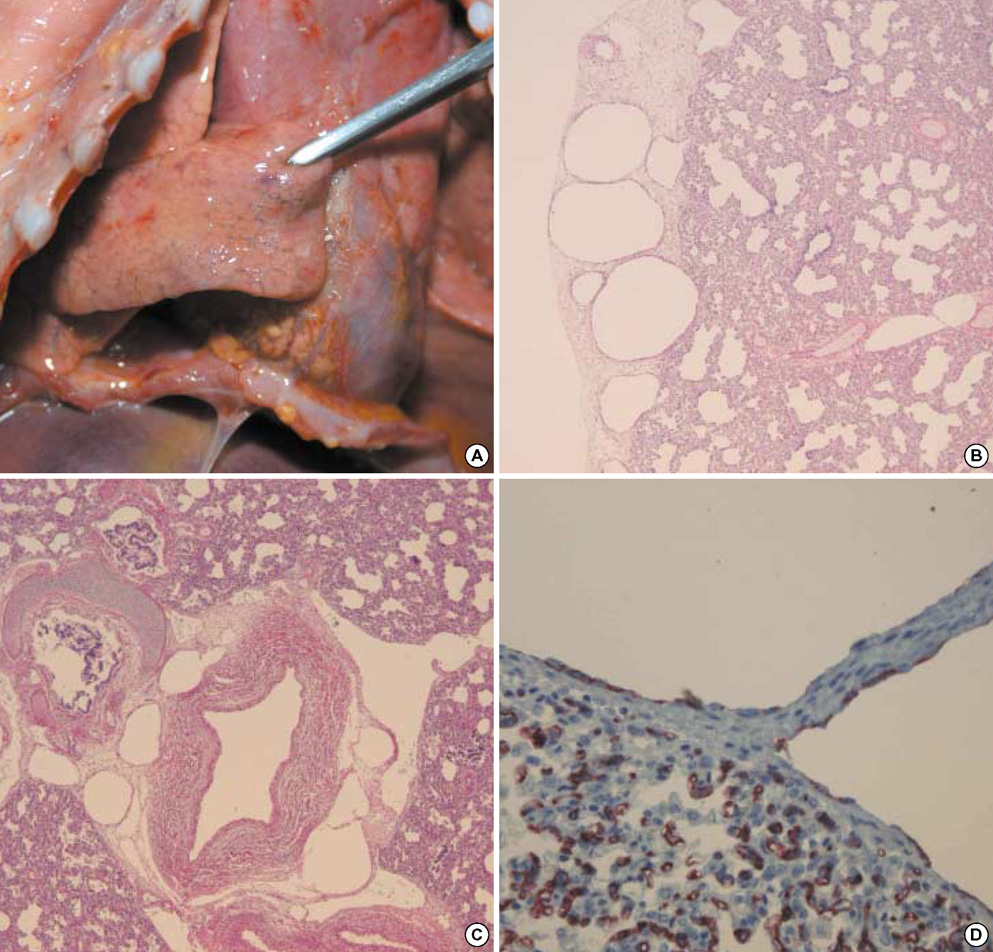
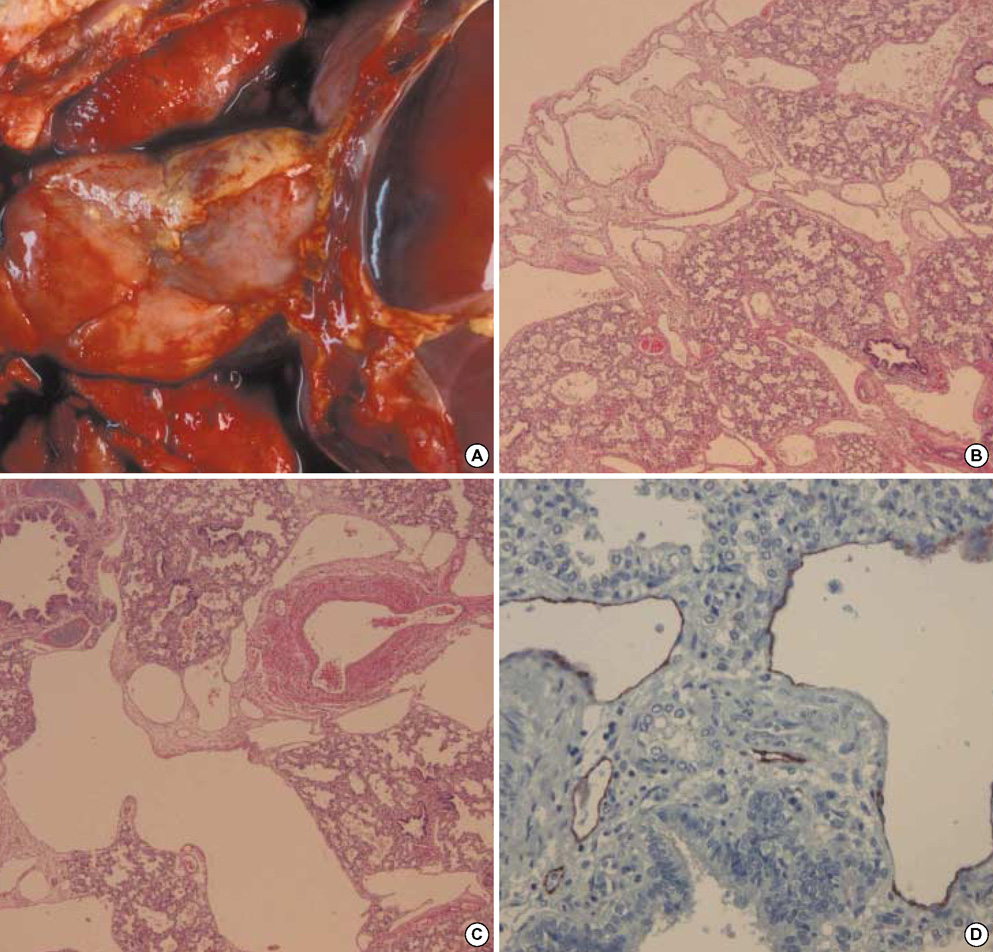
Clinico-pathological Characteristics of Congenital Pulmonary Lymphangiectasis: Report of Two Cases
- Affiliations
-
- 1Department of Forensic Medicine, Western District Office, National Institute of Scientific Investigation, Jangseong, Korea.
- 2Department of Pathology, Wonju College of Medicine, Yonsei University, Wonju, Korea. soonheej@yonsei.ac.kr
- KMID: 1127098
- DOI: http://doi.org/10.3346/jkms.2007.22.4.740
Abstract
- Congenital pulmonary lymphangiectasis (CPL) is a rare, poorly documented disease, characterized by abnormal dilatation of pulmonary lymphatics without lymphatic proliferation. This disease is seen almost exclusively in infancy and early childhood. It can usually be divided into primary (congenital) and secondary forms. The primary form presents in neonates, and the patients mostly die due to the respiratory distress, shortly after birth. The authors experienced two cases of primary CPL in a 13-day-old male neonate and a one-day-old male neonate, showing prominent lymphatic dilatation in the septal, subpleural, and peri-bronchial tissue throughout both lungs. The latter case was associated with congenital cardiac anomaly including single ventricle. These are unique cases of CPL in Korea of which the diagnosis was established through post-mortem examination. Therefore, the authors report these two cases with primary CPL with a review of the literature.
MeSH Terms
Figure
Reference
-
1. France NE, Brown RJ. Congenital pulmonary lymphangiectasis: report of 11 examples with special reference to cardiovascular findings. Arch Dis Child. 1971. 46:528–532.
Article2. Hilliard RI, Mckendry JB, Philips MJ. Congenital abnormalities of the lymphatic system: a new clinical classification. Pediatrics. 1990. 86:988–994.3. Tazelaar HD, Kerr D, Yousem SA, Saldana MJ, Langston C, Colby TV. Diffuse pulmonary lymphangiomatosis. Hum Pathol. 1993. 24:1313–1322.
Article4. Faul JL, Berry GJ, Colby TV, Ruoss SJ, Walter MB, Rosen GD, Raffin TA. Thoracic lymphangiomas, lymphangiectasis, lymphangiomatosis, and lymphatic dysplasia syndrome. Am J Respir Crit Care Med. 2000. 161:1037–1046.
Article5. Bouchard S, Di Lorenzo M, Youssef S, Simard P, Lapierre JG. Pulmonary lymphangiectasia revisited. J Pediatr Surg. 2000. 35:796–800.
Article6. Scully RE, Mark EJ, McNeely WF, McNeely BU. Case records of the massachusetts general hospital: weekly clinicopathological exercises case 13-1992. N Engl J Med. 1992. 326:875–884.7. Brown M, Pysher T, Coffin CM. Lymphangioma and congenital pulmonary lymphangiectasis: a histologic, immunohistochemical, and clinicopathologic comparison. Mod Pathol. 1999. 12:569–575.8. Rettwitz-Volk W, Schlösser R, Ahrens P, Hörlin A. Congenital unilobar pulmonary lymphangiectasis. Pediatr Pulmonol. 1999. 27:290–292.
Article9. Hagemann C, Berger TM. Images in clinical medicine: congenital pulmonary lymphangiectasia. N Engl J Med. 2003. 349:e21.10. Hirano H, Nishigami T, Okimura A, Nakasho K, Uematsu K. Autopsy case of congenital pulmonary lymphangiectasis. Pathol Int. 2004. 54:532–536.
Article11. Nobre LF, Müller NL, de Souza AS Jr, Marchiori E, Souza IV. Congenital pulmonary lymphangiectasia: CT and pathologic findings. J Thorac Imaging. 2004. 19:56–59.12. Kim CH, Kim SH, Park SE, Park JH. A case of pulmonary lympha-ngiectasis. J Korean Pediatr Soc. 1998. 41:715–718.13. Kim MH, Lee JK, Chun OB, Yoo BH, Yoo JH. A case of pulmonary lymphangiectasis associated with chylothorax. J Korean Pediatr Soc. 1987. 30:422–426.14. Lee SY, Yang SR, Lee KR. Congenital pulmonary lymphangiectasia with chylothorax. Asian Cardiovasc Thorac Ann. 2002. 10:76–77.
Article15. Noonan JA, Walters LR, Reeves JT. Congenital pulmonary lymphangiectasis. Am J Dis Child. 1970. 120:314–319.
Article16. Laurence KM. Congenital pulmonary cystic lymphangiectasis. J Path Bact. 1955. 70:325–330.
Article17. Jacquemont S, Barbarot S, Boceno M, Stalder JF, David A. Familial congenital pulmonary lymphangectasia, non-immune hydrops fetalis, facial and lower limb lymphedema: confirmation of Njolstad's report. Am J Med Genet. 2000. 93:264–268.
Article18. Fryns JP, Moerman P. 46,XY/46,XX mosaicism and congenital pulmonary lymphangiectasis with chylothorax. Am J Med Genet. 1993. 47:934–935.
Article19. Katzenstein AL, Askin FB. Katzenstein and Askin's surgical pathology of non-neoplastic lung disease. 1997. 3rd ed. Philadelphia: W.B. Saunders Company;380–381.20. Fukunaga M. Expression of D2-40 in lymphatic endothelium of normal tissues and in vascular tumors. Histopathology. 2005. 46:396–402.