J Korean Med Sci.
2007 Aug;22(4):646-651. 10.3346/jkms.2007.22.4.646.
Postoperative Changes in Paraspinal Muscle Volume: Comparison between Paramedian Interfascial and Midline Approaches for Lumbar Fusion
- Affiliations
-
- 1Department of Neurosurgery , College of Medicine, Chung-Ang University, Seoul, Korea. ybkim1218@cau.ac.kr
- 2Department of Diagnotic Radiology, College of Medicine, Chung-Ang University, Seoul, Korea.
- KMID: 1127080
- DOI: http://doi.org/10.3346/jkms.2007.22.4.646
Abstract
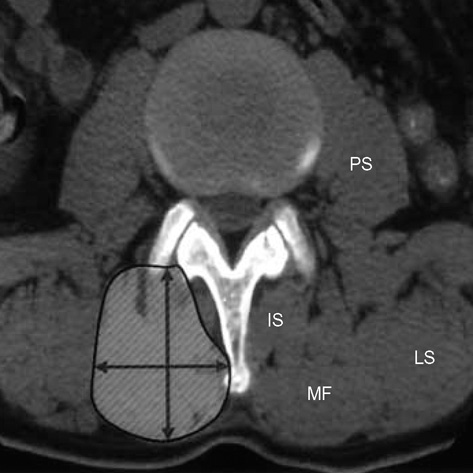
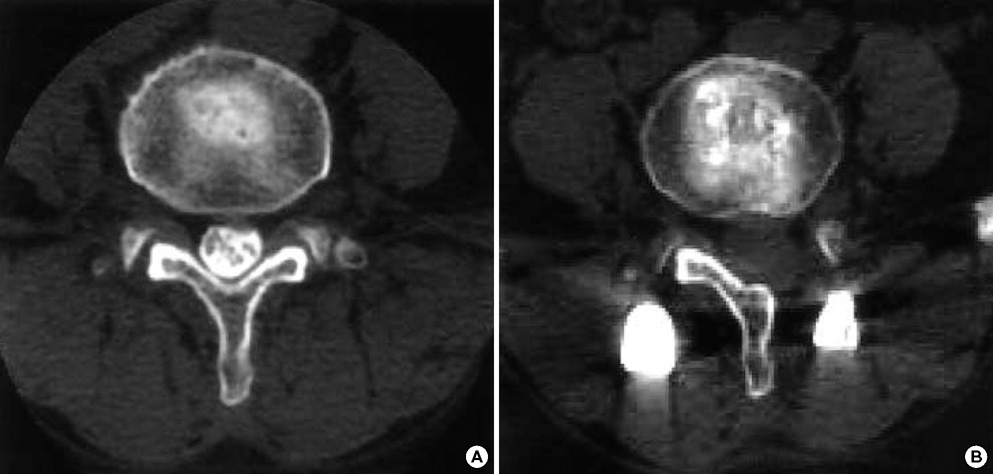
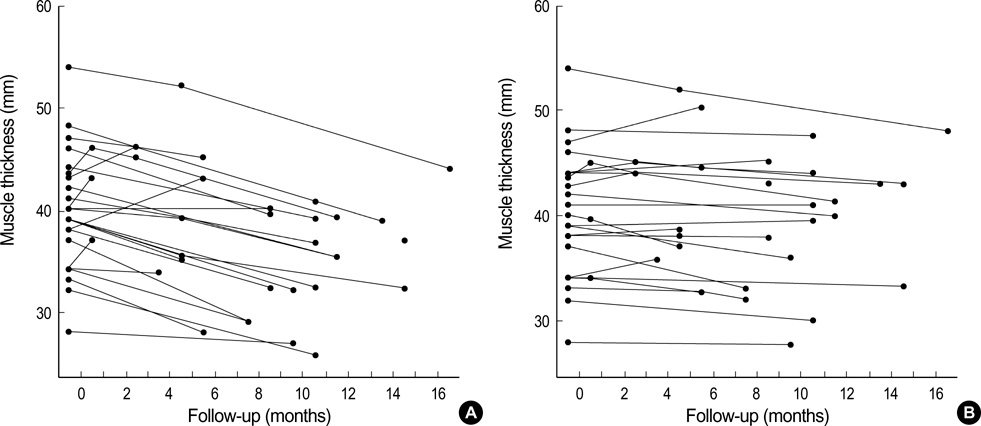
- In this study, we compared the paramedian interfascial approach (PIA) and the traditional midline approach (MA) for lumbar fusion to determine which approach resulted in the least amount of postoperative back muscle atrophy. We performed unilateral transforaminal posterior lumbar interbody fusion via MA on the symptomatic side and pedicle screw fixation via PIA on the other side in the same patient. We evaluated the damage to the paraspinal muscle after MA and PIA by measuring the preoperative and postoperative paraspinal muscle volume in 26 patients. The preoperative and postoperative cross-sectional area, thickness, and width of the multifidus muscle were measured by computed tomography. The degree of postoperative paraspinal muscle atrophy was significantly greater on the MA side than on the contralateral PIA side (-20.7% and -4.8%, respectively, p<0.01). In conclusion, the PIA for lumbar fusion yielded successful outcomes for the preservation of paraspinal muscle in these 26 patients. We suggest that the success of PIA is due to less manipulation and retraction of the paraspinal muscle and further studies on this technique may help confirm whether less muscle injury has positive effects on the long-term clinical outcome.
MeSH Terms
-
Adult
Aged
*Bone Screws
Female
Humans
Lumbar Vertebrae/*surgery
Male
Middle Aged
Muscle, Skeletal/pathology
Muscular Atrophy/etiology/pathology
Postoperative Complications/etiology/pathology
Reproducibility of Results
Retrospective Studies
Spinal Fusion/adverse effects/instrumentation/*methods
Tomography, X-Ray Computed
Figure
Cited by 3 articles
-
The Location of Multifidus Atrophy in Patients With a Single Level, Unilateral Lumbar Radiculopathy
Jung-Il Kang, Sun-Yu Kim, Jin-Hyun Kim, Hyun Bang, In-Sik Lee
Ann Rehabil Med. 2013;37(4):498-504. doi: 10.5535/arm.2013.37.4.498.Back Muscle Changes after Pedicle Based Dynamic Stabilization
Kyung Yun Moon, Soo-Eon Lee, Ki-Jeong Kim, Seung-Jae Hyun, Hyun-Jib Kim, Tae-Ahn Jahng
J Korean Neurosurg Soc. 2013;53(3):174-179. doi: 10.3340/jkns.2013.53.3.174.Sarcopenia and Neurosurgery
Seung Won Park
J Korean Neurosurg Soc. 2014;56(2):79-85. doi: 10.3340/jkns.2014.56.2.79.
Reference
-
1. Harris BM, Hilibrand AS, Savas PE, Pellegrino A, Vaccaro AR, Siegler S, Albert TJ. Transforaminal lumbar interbody fusion: the effect of various instrumentation techniques on the flexibility of the lumbar spine. Spine. 2004. 29:E65–E70.2. Suwa H, Hanakita J, Ohshita N, Gotoh K, Matsuoka N, Morizane A. Postoperative changes in paraspinal muscle thickness after various lumbar back surgery procedures. Neurol Med Chir (Tokyo). 2000. 40:151–154.
Article3. Fritzell P, Hagg O, Wessberg P, Nordwall A. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine. 2002. 27:1131–1141.4. Pradhan BB, Nassar JA, Delamarter RB, Wang JC. Single-level lumbar spine fusion: a comparison of anterior and posterior approaches. J Spinal Disord Tech. 2002. 15:355–361.
Article5. Taylor H, McGregor AH, Medhi-Zadeh S, Richards S, Kahn N, Zadeh JA, Hughes SP. The impact of selfretaining retractors on the paraspinal muscles during posterior spinal surgery. Spine. 2002. 27:2758–2762.
Article6. Vialle R, Court C, Khouri N, Olivier E, Miladi L, Tassin JL, Defives T, Dubousset J. Anatomical study of the paraspinal approach to the lumbar spine. Eur Spine J. 2005. 14:366–371.
Article7. Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993. 18:575–581.
Article8. Foley KT, Holly LT, Schwender JD. Minimally invasive lumbar fusion. Spine. 2003. 28:26–35.
Article9. Kim SW, Shin H. Simultaneous paraspinal and midline Approach for upper lumbar disc herniation: technique to prevent lamina fracture. J Korean Neurosurg Soc. 2005. 38:111–115.10. Harms J, Jeszensky D. The unilateral transforaminal approach for posterior lumbar interbody fusion. Orthop Traumatol. 1998. 6:88–99.11. Boelderl A, Daniaux H, Kathrein A, Maurer H. Danger of damaging the medial branches of the posterior rami of spinal nerves during a dorsomedian approach to the spine. Clinical Anatomy. 2002. 15:77–81.
Article12. Stevens KJ, Spenciner DB, Griffiths KL, Kim KD, Zwienenberg-Lee M, Alamin T, Bammer R. Comparison of minimally invasive and conventional open posterolateral lumbar fusion using magnetic resonance imaging and retraction pressure studies. J Spinal Disord Tech. 2006. 19:77–86.
Article13. Fritzell P, Hagg O, Wessberg P, Nordwall A. Chronic low back pain and fusion: a comparison of three surgical techniques: a prospective multicenter randomized study from the Swedish lumbar spine study group. Spine. 2002. 27:1131–1141.14. Styf JR, Willen J. The effects of external compression by three different retractors on pressure in the erector spine muscles during and after posterior lumbar spine surgery in humans. Spine. 1998. 23:354–358.
Article15. Datta G, Gnanalingham KK, Peterson D, Mendoza N, O'Neill K, Van Dellen J, McGregor A, Hughes SP. Back pain and disability after lumbar laminectomy: is there a relationship to muscle retraction? Neurosurgery. 2004. 54:1413–1420.
Article16. Taylor H, McGregor AH, Medhi-Zadeh S, Richards S, Kahn N, Zadeh JA, Hughes SP. The impact of selfretaining retractors on the paraspinal muscles during posterior spinal surgery. Spine. 2002. 27:2758–2762.
Article17. Pradhan BB, Nassar JA, Delamarter RB, Wang JC. Single-level lumbar spine fusion: a comparison of anterior and posterior approaches. J Spinal Disord Tech. 2002. 15:355–361.
Article18. Macintosh JE, Bogduk N. The biomechanics of the lumbar multifidus. Clin Biomech. 1986. 1:205–213.
Article19. Macintosh JE, Bogduk N. The morphology of the lumbar erector spinae. Spine. 1987. 12:658–668.20. Wilke HJ, Wolf S, Claes LE, Arand M, Wiesend A. Stability increase of the lumbar spine with different muscle groups: a biomechanical in vitro study. Spine. 1995. 20:192–198.21. Sihvonen T, Herno A, Paljarvi L, Airaksinen O, Partanen J, Tapaninaho A. Local denervation atrophy of paraspinal muscles in postoperative failed back syndrome. Spine. 1993. 18:575–581.
Article22. Weiner BK, Walker M, Brower RS, McCulloch JA. Microdecompression for lumbar spinal canal stenosis. Spine. 1999. 24:2268–2272.
Article23. Gejo R, Matsui H, Kawaguchi Y, Ishihara H, Tsuji H. Serial changes in trunk muscle performance after posterior lumbar surgery. Spine. 1999. 24:1023–1028.
Article24. Kawaguchi Y, Matsui H, Tsuji H. Changes in serum creatine phosphokinase MM isoenzyme after lumbar spine surgery. Spine. 1997. 22:1018–1023.
Article25. Wiltse LL, Spencer CW. New uses and refinements of the paraspinal approach to the lumbar spine. Spine. 1988. 13:696–706.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- The Difference of Success Rate between the Midline Approach and the Paramedian Approach of Spinal Anesthesia in each of Flexed Patients and Straightened Patients
- Back Muscle Changes after Pedicle Based Dynamic Stabilization
- Comparison of Depth of Puncture Needle and Difficulty of Puncture in Spinal Anesthesia by Midline or Paramedian Approach in Korean Adults
- Analysis of Factors Contributing to Postoperative Spinal Instability after Lumbar Decompression for Spinal Stenosis
- The Quantitative Analysis of Back Muscle Degeneration after Posterior Lumbar Fusion: Comparison of Minimally Invasive and Conventional Open Surgery