Korean J Ophthalmol.
2009 Mar;23(1):49-52. 10.3341/kjo.2009.23.1.49.
A Choroidal Schwannoma Confirmed by Surgical Excision
- Affiliations
-
- 1Siloam Eye Hospital, Seoul, Korea.
- 2The Institute of Vision Research, Department of Ophthalmology, Yonsei University College of Medicine, Seoul, Korea. sunglee@yuhs.ac
- KMID: 1115653
- DOI: http://doi.org/10.3341/kjo.2009.23.1.49
Abstract
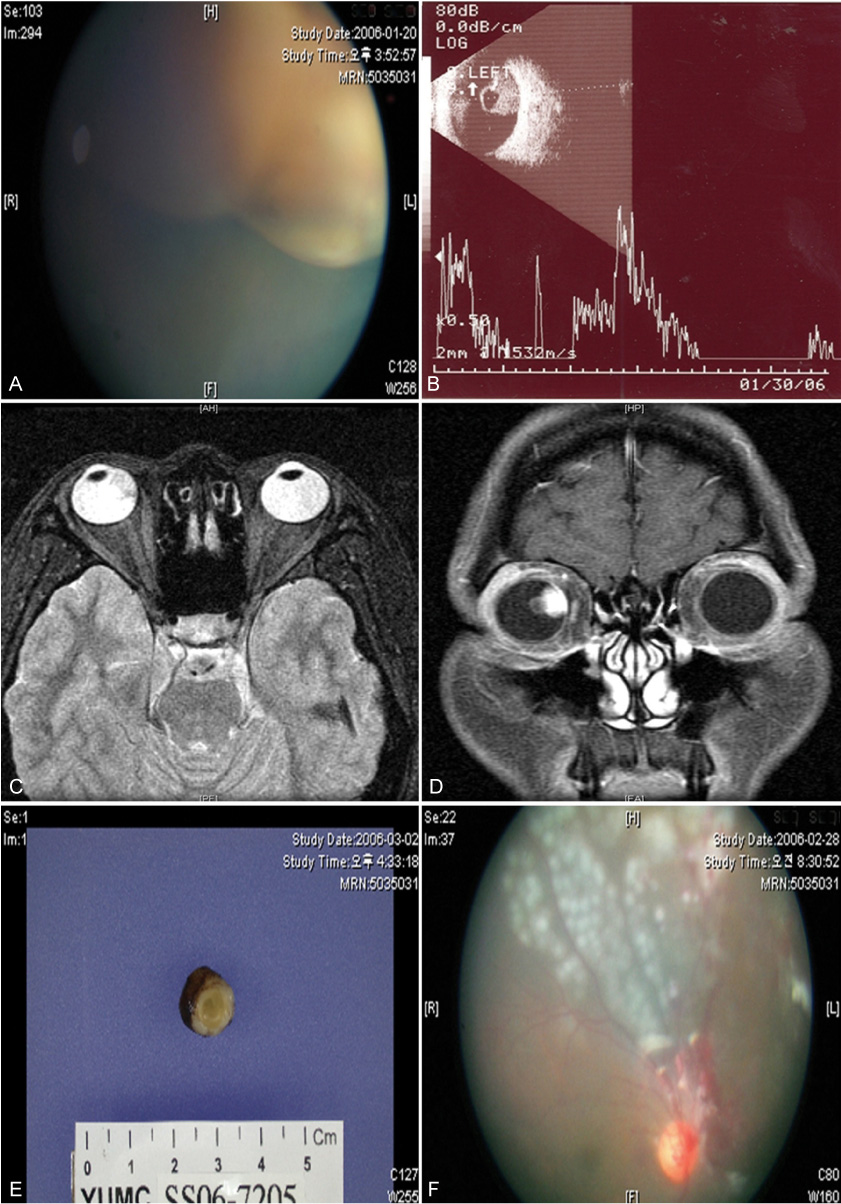
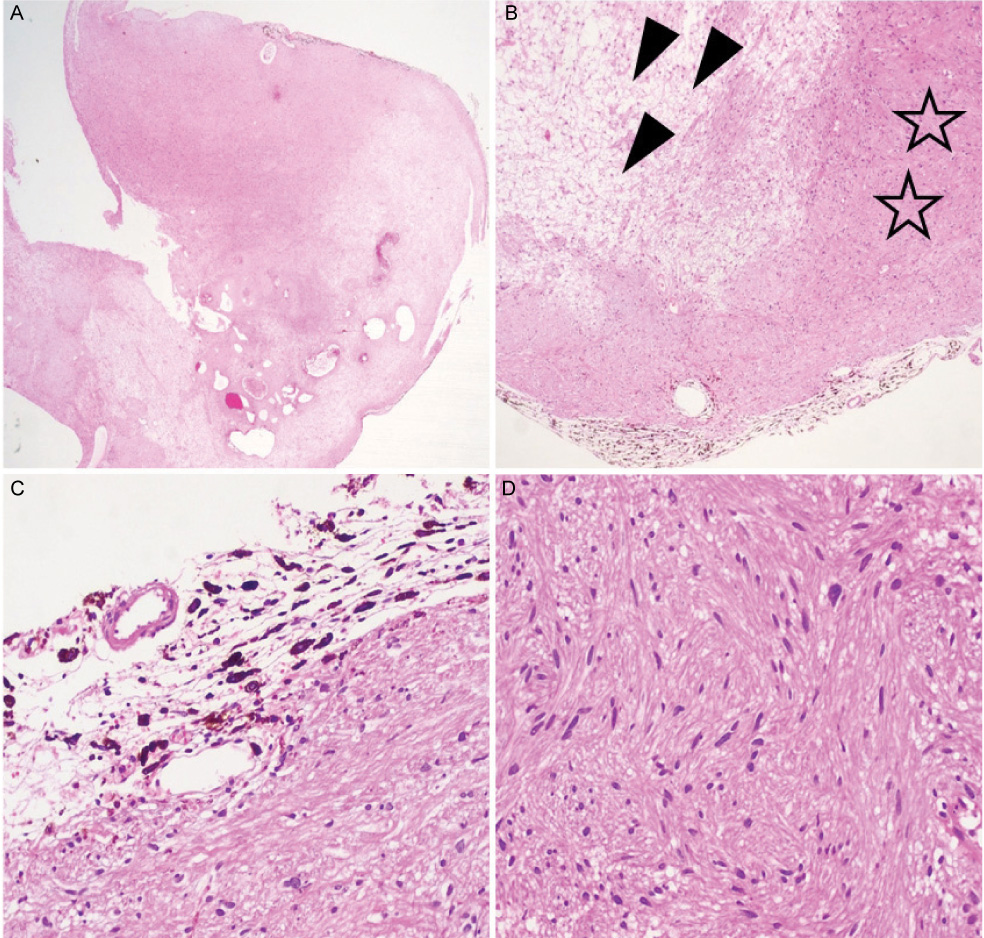
- Schwannomas rarely present as intraocular tumors and are often misdiagnosed as malignant melanoma. We describe a choroidal schwannoma confirmed by sclerouvectomy. A 30-year-old woman presented with a large nonpigmented intraocular mass of the choroid in the right eye and underwent surgical excision by sclerouvectomy. Histologically, the tumor was composed of a mixture of cellular solid components (Antoni A) and loose myxoid components (Antoni B). The tumor was eventually diagnosed as a schwannoma. Currently available ancillary studies are still of little value in definitively differentiating schwannomas from other choroidal tumors. In the case of atypical findings for a malignant melanoma, a benign neoplasm should be included in the differential diagnosis. This patient avoided enucleation by first having the mass excised. We are unaware of previous reports in which a choroidal schwannoma was diagnosed by surgical excision.
Keyword
MeSH Terms
Figure
Reference
-
1. Shields JA, Sanborn GE, Kurz GH, et al. Benign peripheral nerve tumor of the choroid : a clinicopathologic correlation and review of the literature. Ophthalmology. 1981. 88:1322–1329.2. Fan JT, Campbell RJ, Robertson DM. A survey of intraocular schwannoma with a case report. Can J Ophthalmol. 1995. 30:37–41.3. Hufnagel TJ, Sears ML, Shapiro M, Kim JH. Ciliary body neurilemoma recurring after 15 years. Graefes Arch Clin Exp Ophthalmol. 1988. 226:443–446.4. Smith PA, Damato BE, Ko MK, Lyness RW. Anterior uveal neurilemmoma: a rare neoplasm simulating malignant melanoma. Br J Ophthalmol. 1987. 71:34–40.5. Matsuo T, Notohara K. Choroidal schwannoma: immunohistochemical and electron-microscopic study. Ophthalmologica. 2000. 214:156–160.6. Lee SH, Hong JS, Choi JH. Choroidal schwannoma. Acta Ophthalmol Scand. 2005. 83:754–756.7. Pineda R 2nd, Urban RC Jr, Bellows AR, Jakbiec FA. Ciliary body neurilemoma. Unusual clinical findings intimating the diagnosis. Ophthalmology. 1995. 102:918–923.8. Kuchle M, Holbach L, Schlotzer-Schrehardt U, Naumann GO. Schwannoma of the ciliary body treated by block excision. Br J Ophthalmol. 1994. 78:397–400.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Schwannoma of the Chorda Tympani Nerve
- Malignant Schwannoma: Report of Two Cases
- A Case of Malignant Schwannoma in the Thoracolumbal Region
- Two Cases of Malignant Schwannoma in Association with Neurofibromatosis
- Schwannoma of the Ulnar Nerve as a Superficial Cutaneous Mass: Surgical Considerations