Yonsei Med J.
2011 Sep;52(5):831-837. 10.3349/ymj.2011.52.5.831.
CT Evaluation of Vocal Cord Paralysis due to Thoracic Diseases: A 10-Year Retrospective Study
- Affiliations
-
- 1Department of Radiology, Uijeongbu St. Mary's Hospital, The Catholic University of Korea College of Medicine, Uijeongbu, Korea.
- 2Department of Otolaryngology-Head and Neck Surgery, Uijeongbu St. Mary's Hospital, The Catholic University of Korea College of Medicine, Uijeongbu, Korea. otojun@catholic.ac.kr
- 3Department of Radiology, Seoul St. Mary's Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea.
- KMID: 1108077
- DOI: http://doi.org/10.3349/ymj.2011.52.5.831
Abstract
- PURPOSE
To discuss computed tomography (CT) evaluation of the etiology of vocal cord paralysis (VCP) due to thoracic diseases.
MATERIALS AND METHODS
From records from the past 10 years at our hospital, we retrospectively reviewed 115 cases of VCP that were evaluated with CT. Of these 115 cases, 36 patients (23 M, 13 F) had VCP due to a condition within the thoracic cavity. From these cases, we collected the following information: sex, age distribution, side of paralysis, symptom onset date, date of diagnosis, imaging, and primary disease. The etiology of VCP was determined using both historical information and diagnostic imaging. Imaging procedures included chest radiograph, CT of neck or chest, and esophagography or esophagoscopy.
RESULTS
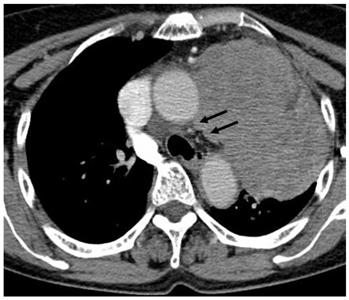
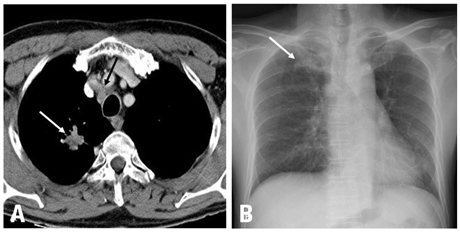
Thirty-three of the 36 patients with thoracic disease had unilateral VCP (21 left, 12 right). Of the primary thoracic diseases, malignancy was the most common (19, 52.8%), with 18 of the 19 malignancies presenting with unilateral VCP. The detected malignant tumors in the chest consisted of thirteen lung cancers, three esophageal cancers, two metastatic tumors, and one mediastinal tumor. We also found other underlying etiologies of VCP, including one aortic arch aneurysm, five iatrogenic, six tuberculosis, one neurofibromatosis, three benign nodes, and one lung collapse. A chest radiograph failed to detect eight of the 19 primary malignancies detected on the CT. Nine patients with lung cancer developed VCP between follow-ups and four of them were diagnosed with a progression of malignancy upon CT evaluation of VCP.
CONCLUSION
CT is helpful for the early detection of primary malignancy or progression of malignancy between follow-ups. Moreover, it can reveal various non-malignant causes of VCP.
Keyword
MeSH Terms
-
Adult
Aged
Aged, 80 and over
Female
Humans
Lung Neoplasms/complications/pathology
Male
Middle Aged
Neoplasm Invasiveness
Recurrent Laryngeal Nerve/pathology
Retrospective Studies
Thoracic Diseases/*complications
Tomography, X-Ray Computed
Tuberculosis, Pulmonary/complications
Vocal Cord Paralysis/*etiology/*radiography
Figure
Reference
-
1. Benninger MS, Gillen JB, Altman JS. Changing etiology of vocal fold immobility. Laryngoscope. 1998. 108:1346–1350.
Article2. Bando H, Nishio T, Bamba H, Uno T, Hisa Y. Vocal fold paralysis as a sign of chest diseases: a 15-year retrospective study. World J Surg. 2006. 30:293–298.
Article3. Furukawa M, Furukawa MK, Ooishi K. Statistical analysis of malignant tumors detected as the cause of vocal cord paralysis. ORL J Otorhinolaryngol Relat Spec. 1994. 56:161–165.
Article4. Glazer HS, Aronberg DJ, Lee JK, Sagel SS. Extralaryngeal causes of vocal cord paralysis: CT evaluation. AJR Am J Roentgenol. 1983. 141:527–531.
Article5. Titche LL. Causes of recurrent laryngeal nerve paralysis. Arch Otolaryngol. 1976. 102:259–261.
Article6. Evans JM, Schucany WG. Hoarseness and cough in a 67-year-old woman. Proc (Bayl Univ Med Cent). 2004. 17:469–472.
Article7. Chen HC, Jen YM, Wang CH, Lee JC, Lin YS. Etiology of vocal cord paralysis. ORL J Otorhinolaryngol Relat Spec. 2007. 69:167–171.
Article8. de Gandt JB. [Recurrent nerve compression]. Acta Otorhinolaryngol Belg. 1970. 24:520–554.9. Terris DJ, Arnstein DP, Nguyen HH. Contemporary evaluation of unilateral vocal cord paralysis. Otolaryngol Head Neck Surg. 1992. 107:84–90.
Article10. Sherani TM, Angelini GD, Passani SP, Butchart EG. Vocal cord paralysis associated with coalworkers' pneumoconiosis and progressive massive fibrosis. Thorax. 1984. 39:683–684.
Article11. Altman JS, Benninger MS. The evaluation of unilateral vocal fold immobility: is chest X-ray enough? J Voice. 1997. 11:364–367.12. Camishion RC, Gibbon JH Jr, Pierucci L Jr. Paralysis of the left recurrent laryngeal nerve secondary to mitral valvular disease. Report of two cases and literature review. Ann Surg. 1966. 163:818–828.
Article13. Che GW, Chen J, Liu LX, Zhou QH. Aortic arch aneurysm rupture into the lung misdiagnosed as lung carcinoma. Can J Surg. 2008. 51:E91–E92.14. Bin HG, Kim MS, Kim SC, Keun JB, Lee JH, Kim SS. Intrathoracic aneurysm of the right subclavian artery presenting with hoarseness: a case report. J Korean Med Sci. 2005. 20:674–676.
Article15. Kokotsakis J, Misthos P, Athanassiou T, Skouteli E, Rontogianni D, Lioulias A. Acute Ortner's syndrome arising from ductus arteriosus aneurysm. Tex Heart Inst J. 2008. 35:216–217.16. Gothi R, Ghonge NP. Case Report: Spontaneous aneurysm of ductus arteriosus: A rare cause of hoarseness of voice in adults. Indian J Radiol Imaging. 2008. 18:322–323.
Article17. Morgan AA, Mourant AJ. Left vocal cord paralysis and dysphagia in mitral valve disease. Br Heart J. 1980. 43:470–473.
Article18. el-Kassimi FA, Ashour M, Vijayaraghavan R. Sarcoidosis presenting as recurrent left laryngeal nerve palsy. Thorax. 1990. 45:565–566.
Article19. Fowler RW, Hetzel MR. Tuberculous mediastinal lymphadenopathy can cause left vocal cord paralysis. Br Med J (Clin Res Ed). 1983. 286:1562.
Article20. Strickland B, Wolverson MK. Intrathoracic vagus nerve tumours. Thorax. 1974. 29:215–222.
Article21. Barondess JA, Pompei P, Schley WS. A study of vocal cord palsy. Trans Am Clin Climatol Assoc. 1986. 97:141–148.22. Ellis PD, Pallister WK. Recurrent laryngeal nerve palsy and endotracheal intubation. J Laryngol Otol. 1975. 89:823–826.
Article23. Holinger LD, Holinger PC, Holinger PH. Etiology of bilateral abductor vocal cord paralysis: a review of 389 cases. Ann Otol Rhinol Laryngol. 1976. 85:428–436.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vocal Cord Paralysis Due to Extralaryngeal Causes: Evaluation with CT1
- Guillain-Barre Syndrome Presenting as Bilateral Vocal Cord Paralysis
- Laryngeal Electromyography: Clinical Application in Vocal Cord Palsy
- A Case of Bilateral Vocal Cord Paralysis from Progressive Supranuclear Palsy
- A Case of Bilateral Vocal Cord Paralysis Due to Subglottic Pressure Injury after Endotracheal Intubation: A Case Report