Yonsei Med J.
2011 Sep;52(5):818-830. 10.3349/ymj.2011.52.5.818.
Limb Angular Deformity Correction Using Dyna-ATC: Surgical Technique, Calculation Method, and Clinical Outcome
- Affiliations
-
- 1Department of Orthopaedic Surgery, Yonsei University College of Medicine, Seoul, Korea. leeks@yuhs.ac
- KMID: 1108076
- DOI: http://doi.org/10.3349/ymj.2011.52.5.818
Abstract
- PURPOSE
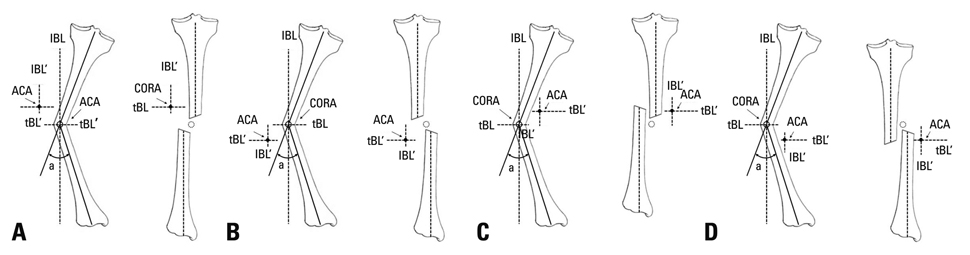
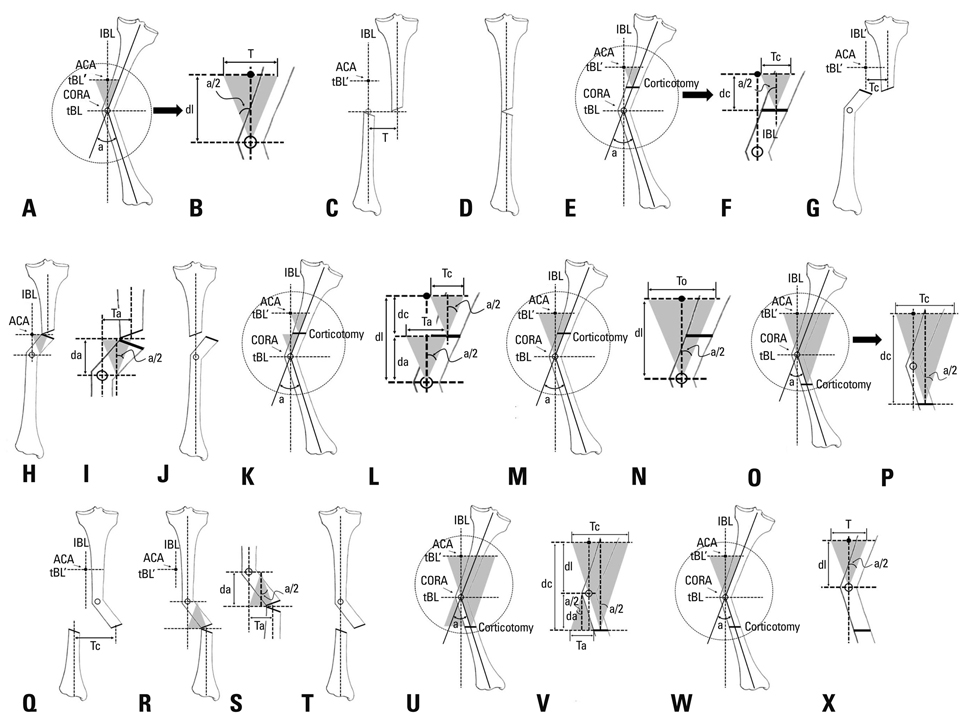
Dyna-ATC is a unilateral external fixator with angulator, lengthener, and translator, which allows for angular correction and compensation of the secondary displacement during angular correction. The purpose of this study is to introduce surgical technique and calculation methods and to evaluate the clinical outcome of angular deformity correction using Dyna-ATC.
MATERIALS AND METHODS
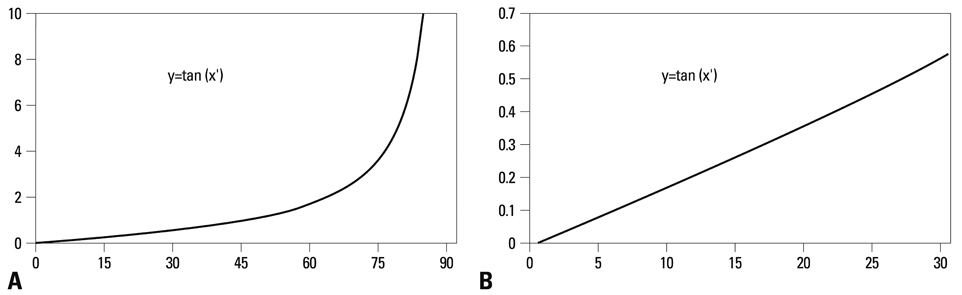
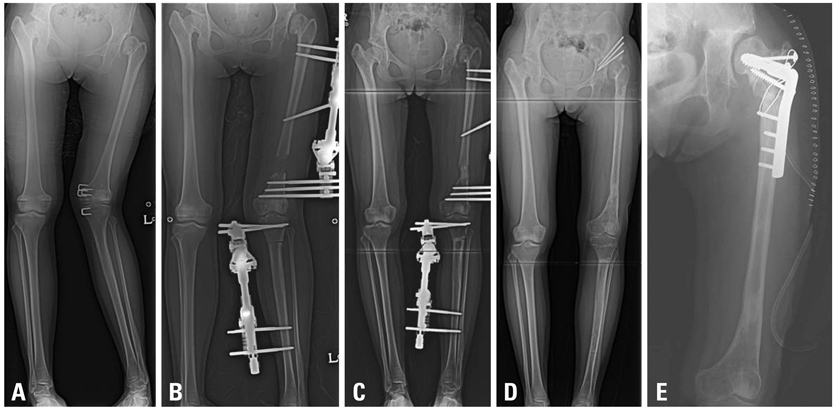
The amounts of secondary displacement were calculated with the distances between axis of correction of angulation, Center of Rotational Angulation, and osteotomy and the amount of angular deformity. The rate of angular correction was determined to distract the corticotomy at 1 mm/day. Clinical and radiographic evaluation was performed on 13 patients who underwent deformity correction using Dyna-ATC. There were 8 proximal tibia vara, 1 tibia valga, 2 varus and 4 valgus deformities on distal femur. One patient underwent pelvic support femoral reconstruction. Concomitant lengthening was combined in all femur cases. Mean age at surgery was 17.5 years (7 to 64).
RESULTS
All but one achieved bony healing and normal alignment with the index procedure. Mean mechanical axis deviation improved from 31.9 mm to 3.0 mm. The average amount of angular correction was 11.0degrees on tibiae and 10.0degrees on femora. The average length gain on femora was 6.4 cm, and the healing index averaged to 1.1 mo/cm. One patient underwent quadricepsplasty and one patient had three augmentation surgeries due to poor new bone formation.
CONCLUSION
We believe that Dyna-ATC is a useful alternative to bulky ring fixators for selective patients with angular deformity less than 30 degrees in the coronal plane around the knee joint.
MeSH Terms
-
Adolescent
Bone Diseases, Developmental/*surgery
Child
*External Fixators
Female
Femur/abnormalities/surgery
Humans
Leg Length Inequality/surgery
Lower Extremity Deformities, Congenital/*surgery
Male
Middle Aged
Osteochondrosis/congenital/surgery
Osteogenesis, Distraction/*instrumentation/methods/statistics & numerical data
Osteotomy
Tibia/abnormalities/surgery
Treatment Outcome
Young Adult
Figure
Reference
-
1. Gilbody J, Thomas G, Ho K. Acute versus gradual correction of idiopathic tibia vara in children: a systematic review. J Pediatr Orthop. 2009. 29:110–114.2. Feldman DS, Madan SS, Ruchelsman DE, Sala DA, Lehman WB. Accuracy of correction of tibia vara: acute versus gradual correction. J Pediatr Orthop. 2006. 26:794–798.3. Kamegaya M, Shinohara Y, Shinada Y. Limb lengthening and correction of angulation deformity: immediate correction by using a unilateral fixator. J Pediatr Orthop. 1996. 16:477–479.
Article4. Noonan KJ, Price CT, Sproul JT, Bright RW. Acute correction and distraction osteogenesis for the malaligned and shortened lower extremity. J Pediatr Orthop. 1998. 18:178–186.
Article5. Behrens F. General theory and principles of external fixation. Clin Orthop Relat Res. 1989. 15–23.
Article6. Herbert AJ, Herzenberg JE, Paley D. A review for pediatricians on limb lengthening and the Ilizarov method. Curr Opin Pediatr. 1995. 7:98–105.7. Noonan KJ, Leyes M, Forriol F, Cañadell J. Distraction osteogenesis of the lower extremity with use of monolateral external fixation. A study of two hundred and sixty-one femora and tibiae. J Bone Joint Surg Am. 1998. 80:793–806.
Article8. Kim YH, Inoue N, Chao EY. Kinematic simulation of fracture reduction and bone deformity correction under unilateral external fixation. J Biomech. 2002. 35:1047–1058.
Article9. Birch JG, Samchukov ML. Use of the Ilizarov method to correct lower limb deformities in children and adolescents. J Am Acad Orthop Surg. 2004. 12:144–154.
Article10. Tsuchiya H, Uehara K, Abdel-Wanis ME, Sakurakichi K, Kabata T, Tomita K. Deformity correction followed by lengthening with the Ilizarov method. Clin Orthop Relat Res. 2002. 176–183.
Article11. Coogan PG, Fox JA, Fitch RD. Treatment of adolescent Blount disease with the circular external fixation device and distraction osteogenesis. J Pediatr Orthop. 1996. 16:450–454.
Article12. McCarthy JJ, Ranade A, Davidson RS. Pediatric deformity correction using a multiaxial correction fixator. Clin Orthop Relat Res. 2008. 466:3011–3017.
Article13. McLawhorn AS, Sherman SL, Blyakher A, Widmann RF. Humeral lengthening and deformity correction with the multiaxial correction system. J Pediatr Orthop B. 2011. 20:111–116.
Article14. Teruhisa Y, Hiroyuki T, Keisuke S, Tamon K, Katsuro T. Gradual correction of limb deformity using the Heidelberg external fixator. Nihonsougaikoteikenkyukaishi. J Jpn Soc Extern Fixat. 2003. 14:47–51.15. Price CT, Scott DS, Greenberg DA. Dynamic axial external fixation in the surgical treatment of tibia vara. J Pediatr Orthop. 1995. 15:236–243.
Article16. Stanitski DF, Srivastava P, Stanitski CL. Correction of proximal tibial deformities in adolescents with the T-Garches external fixator. J Pediatr Orthop. 1998. 18:512–517.
Article17. Paley D, Tetsworth K. Mechanical axis deviation of the lower limbs. Preoperative planning of uniapical angular deformities of the tibia or femur. Clin Orthop Relat Res. 1992. 48–64.18. Paley D, Herzenberg JE, Tetsworth K, McKie J, Bhave A. Deformity planning for frontal and sagittal plane corrective osteotomies. Orthop Clin North Am. 1994. 25:425–465.
Article19. Paley D. Problems, obstacles, and complications of limb lengthening by the Ilizarov technique. Clin Orthop Relat Res. 1990. 81–104.
Article20. Gladbach B, Heijens E, Pfeil J, Paley D. Calculation and correction of secondary translation deformities and secondary length deformities. Orthopedics. 2004. 27:760–766.
Article21. Paley D. Extensive limb lengthening. Baltimore Method. In : 18th Annual Baltimore limb deformity course; 2008, Aug 30; Baltimore, MD.22. Fadel M, Hosny G. The Taylor spatial frame for deformity correction in the lower limbs. Int Orthop. 2005. 29:125–129.
Article23. Feldman DS, Madan SS, Koval KJ, van Bosse HJ, Bazzi J, Lehman WB. Correction of tibia vara with six-axis deformity analysis and the Taylor Spatial Frame. J Pediatr Orthop. 2003. 23:387–391.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Change in Effective Leg Length after Angular Deformity Correction by Hemiepiphyseal Stapling
- Prognostic Factors of Physeal Bar Resection and Fat Graft Interposition in the Treatment of Partial Physeal Arrest
- Ilizarov Technique for Simulataneous correction of Angular and Rotational Deformities : The Use of Inclined Hinges with Universal Joints
- Lengthening & Deformity Correction in Upper Extremities by the Ilizarov Method
- Angular Deformity Correction by Asymmetrical Physeal Supression in Children