Yonsei Med J.
2011 Jan;52(1):33-38. 10.3349/ymj.2011.52.1.33.
Clinical and Echocardiographic Findings of Newly Diagnosed Acute Decompensated Heart Failure in Elderly Patients
- Affiliations
-
- 1Cardiology Division, Yonsei Cardiovascular Hospital and Cardiovascular Research Institute, Seoul, Korea. smkang@yuhs.ac
- 2Brain Korea 21 Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 1106434
- DOI: http://doi.org/10.3349/ymj.2011.52.1.33
Abstract
- PURPOSE
Elderly patients (pts) (EPs; > or = 65 years old) with newly diagnosed-acute decompensated heart failure (ND-ADHF) have not yet been studied. The aim of the present study was to investigate clinical characteristics, including echocardiographic findings and prognosis, for EPs with ND-ADHF and to compare those with non-elderly pts (NEPs).
MATERIALS AND METHODS
We retrospectively investigated 256 pts (144 males, 63.0 +/- 14.8 years old) who were admitted to our hospital between January 2005 and March 2009 with ND-ADHF. Clinical characteristics and echocardiographic parameters were analyzed in EPs (n = 135, 58 males) and NEPs (n = 121, 86 males).
RESULTS
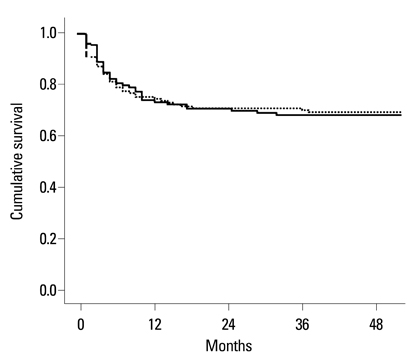
In intergroup comparison, female gender, diabetes mellitus, previous stroke and hypertension were more common in EPs. Body mass index (22.3 +/- 4.5 vs. 24.0 +/- 4.4 kg/m2), estimated glomerular filtration rate (54.8 +/- 24.3 vs. 69.2 +/- 30.7 mL/min/m2), C-reactive protein (28.5 +/- 46.9 vs. 7.6 +/- 11.6 mg/dL), hemoglobin (12.3 +/- 2.1 vs. 13.6 +/- 2.3 g/dL) and N-terminal pro-brain natriuretic peptide level (10,538.2 +/- 10,942.3 vs. 6,771.0 +/- 8,964.7 pg/mL) were significantly different (p < 0.05 for all). Early mitral inflow velocity to early diastolic mitral annular velocity (E/E') was significantly higher in EPs than in NEPs (21.2 +/- 9.4 vs. 18.0 +/- 8.9, p < 0.05). During follow-up (44.7 +/- 14.5 months), there were no significant differences in in-hospital mortality, re-hospitalization and cardiovascular mortality between EPs and NEPs (p = NS for all).
CONCLUSION
EPs with ND-ADHF have different clinical characteristics and higher LV filling pressure when compared with NEPs. However, the clinical outcomes for NEPs with ND-ADHF are not necessarily more favorable than those for EPs.
MeSH Terms
Figure
Reference
-
1. Havranek EP, Masoudi FA, Westfall KA, Wolfe P, Ordin DL, Krumholz HM. Spectrum of heart failure in older patients: results from the National Heart Failure project. Am Heart J. 2002. 143:412–417.
Article2. Miani D, Fresco C, Lucci D, Albanese MC, Gonzini L, Fioretti PM, et al. Clinical characteristics, management, and prognosis of octogenarians with acute heart failure admitted to cardiology wards: results from the Italian Survey on Acute Heart Failure. Am Heart J. 2009. 158:126–132.
Article3. Fonarow GC. Epidemiology and risk stratification in acute heart failure. Am Heart J. 2008. 155:200–207.
Article4. Coats AJ. Is preventive medicine responsible for the increasing prevalence of heart failure? Lancet. 1998. 352:Suppl 1. SI39–SI41.
Article5. Heiat A, Gross CP, Krumholz HM. Representation of the elderly, women, and minorities in heart failure clinical trials. Arch Intern Med. 2002. 162:1682–1688.
Article6. Kannel WB. Epidemiology and prevention of cardiac failure: Framingham Study insights. Eur Heart J. 1987. 8:Suppl F. 23–26.
Article7. Kannel WB, Belanger AJ. Epidemiology of heart failure. Am Heart J. 1991. 121:951–957.
Article8. Gambassi G, Forman DE, Lapane KL, Mor V, Sgadari A, Lipsitz LA, et al. The SAGE Study Group. Management of heart failure among very old persons living in long-term care: has the voice of trials spread? Am Heart J. 2000. 139:85–93.
Article9. McMurray JJ, Pfeffer MA. Heart failure. Lancet. 2005. 365:1877–1889.
Article10. Hunt SA. American College of Cardiology; American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). ACC/AHA 2005 guideline update for the diagnosis and management of chronic heart failure in the adult: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines (Writing Committee to Update the 2001 Guidelines for the Evaluation and Management of Heart Failure). J Am Coll Cardiol. 2005. 46:e1–e82.11. Lang RM, Bierig M, Devereux RB, Flachskampf FA, Foster E, Pellikka PA, et al. Recommendations for chamber quantification: a report from the American Society of Echocardiography's Guidelines and Standards Committee and the Chamber Quantification Writing Group, developed in conjunction with the European Association of Echocardiography, a branch of the European Society of Cardiology. J Am Soc Echocardiogr. 2005. 18:1440–1463.
Article12. Haldeman GA, Croft JB, Giles WH, Rashidee A. Hospitalization of patients with heart failure: National Hospital Discharge Survey, 1985 to 1995. Am Heart J. 1999. 137:352–360.
Article13. Parmley WW. Do we practice geriatric cardiology? J Am Coll Cardiol. 1997. 29:217–218.14. Lavie CJ, Milani RV, Ventura HO. Obesity and cardiovascular disease: risk factor, paradox, and impact of weight loss. J Am Coll Cardiol. 2009. 53:1925–1932.15. Horwich TB, Fonarow GC, Hamilton MA, MacLellan WR, Woo MA, Tillisch JH. The relationship between obesity and mortality in patients with heart failure. J Am Coll Cardiol. 2001. 38:789–795.
Article16. Mahjoub H, Rusinaru D, Soulière V, Durier C, Peltier M, Tribouilloy C. Long-term survival in patients older than 80 years hospitalised for heart failure. A 5-year prospective study. Eur J Heart Fail. 2008. 10:78–84.
Article17. Lien CT, Gillespie ND, Struthers AD, McMurdo ME. Heart failure in frail elderly patients: diagnostic difficulties, co-morbidities, polypharmacy and treatment dilemmas. Eur J Heart Fail. 2002. 4:91–98.
Article18. Daniels LB, Maisel AS. Natriuretic peptides. J Am Coll Cardiol. 2007. 50:2357–2368.
Article19. Kubler P, Jankowska EA, Majda J, Reczuch K, Banasiak W, Ponikowski P. Lack of decrease in plasma N-terminal pro-brain natriuretic peptide identifies acute heart failure patients with very poor outcome. Int J Cardiol. 2008. 129:373–378.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Medical Treatment of Acute Decompensated Heart Failure Syndrome
- Clinical Impact of Worsening Renal Function in Elderly Patients with Acute Decompensated Heart Failure
- Clinical and Imaging Parameters Associated With Impaired Kidney Function in Patients With Acute Decompensated Heart Failure With Reduced Ejection Fraction
- The Heart in Acute Glomerulonephritis: An Echocardiographic Study
- Worsening Renal Function during Acute Decompensated Heart Failure: A Bad Signal Never to Ignore