Yonsei Med J.
2009 Oct;50(5):650-655. 10.3349/ymj.2009.50.5.650.
Variability of Response Time as a Predictor of Methylphenidate Treatment Response in Korean Children with Attention Deficit Hyperactivity Disorder
- Affiliations
-
- 1Department of Psychiatry, Sungkyunkwan University School of Medicine, Kangbuk Samsung Hospital, Seoul, Korea. ntour@unitel.co.kr
- 2Department of Psychiatry and The Institute of Behavioral Science in Medicine, Yonsei University College of Medicine, Seoul, Korea.
- 3Department of Psychiatry, Seoul National University Hospital, Seoul, Korea.
- 4Department of Psychiatry, Sungkyunkwan University School of Medicine, Samsung Medical Center, Seoul, Korea.
- 5Department of Child Welfare, Sookmyung Women's University, Seoul, Korea.
- 6Department of Psychiatry, Kwandong University College of Medicine, Myong-Ji Hospital, Goyang, Korea.
- 7Department of Psychiatry, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 1103818
- DOI: http://doi.org/10.3349/ymj.2009.50.5.650
Abstract
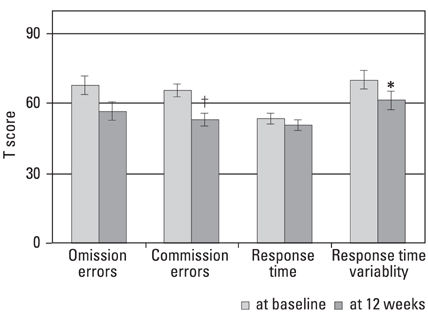
- PURPOSE
Methylphenidate (MPH) is an effective medication for the treatment of attention deficit hyperactivity disorder (ADHD). However, about 30% of patients do not respond to or are unable to tolerate MPH. Based on previous findings, we hypothesized that great variability in response time (RT) among Korean children with ADHD on a computerized continuous performance attention test would be related to poor MPH treatment response. MATERIALS AND METHODS: Children (ages 6-18 years) with ADHD were recruited for a prospective 12-week, open-labeled, multicenter study to examine optimal dosage of OROS methylphenidate. Of the 144 subjects selected, 28 dropped out due to adverse events, medication noncompliance, or follow-up loss, and an additional 26 subjects with comorbid disorders were excluded from statistical analyses. We defined 'responders' as subjects who received a score of less than 18 on the attention deficit hyperactivity disorder rating scale (ARS; Korean version, K-ARS) and a score of 1 or 2 on the Clinical Global Impression-Improvement scale (CGI-I). RT variability was assessed with the ADHD diagnostic system (ADS). RESULTS: Fifty-nine (67%) subjects responded to MPH treatment. The non-responders showed greater RT variability at baseline (Mann Whitney U = 577.0, p < 0.01). Baseline RT variability was a significant predictor of MPH response (Nagelkerke R2 = 0.136, p < 0.01). It predicted 94.9% of responder, 17.2% of non-responder and 69.3% of overall group. CONCLUSION: High RT variability may predict poor response to MPH treatment in children with ADHD.
Keyword
MeSH Terms
Figure
Reference
-
1. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 2000. 4th ed. Washington DC: American Psychiatric Association.2. Barkley RA. Barkley RA, editor. Associated Cognitive, Developmental, and Health Problems. Attention-Deficit Hyperactivity Disorder: a Handbook for Diagnosis and Treatment. 2006. 3rd ed. New York: The Guilford Press;123–183.3. Barkley RA. Comorbid Disorders, Social and Family Adjustment, and Subtyping. Attention-Deficit Hyperactivity Disorder: a Handbook for Diagnosis and Treatment. 2006. 3rd ed. New York: The Guilford Press;184–218.4. Mannuzza S, Klein RG, Bessler A, Malloy P, LaPadula M. Adult outcome of hyperactive boys. Educational achievement, occupational rank, and psychiatric status. Arch Gen Psychiatry. 1993. 50:565–576.5. Loeber R, Dishion T. Early predictors of male delinquency: a review. Psychol Bull. 1983. 94:68–99.6. Gittelman R, Mannuzza S, Shenker R, Bonagura N. Hyperactive boys almost grown up. I. Psychiatric status. Arch Gen Psychiatry. 1985. 42:937–947.7. Barkley RA, Fischer M, Smallish L, Fletcher K. Young adult follow-up of hyperactive children: antisocial activities and drug use. J Child Psychol Psychiatry. 2004. 45:195–211.8. Morrison J. Adult psychiatric disorders in parents of hyperactive children. Am J Psychiatry. 1980. 137:825–827.9. Swanson JM, Wigal SB, Wigal T, Sonuga-Barke E, Greenhill LL, Biederman J, et al. A comparison of once-daily extended-release methylphenidate formulations in children with attention-deficit/hyperactivity disorder in the laboratory school (the Comacs Study). Pediatrics. 2004. 113:e206–e216.
Article10. Biederman J. Pharmacotherapy for attention-deficit/hyperactivity disorder (ADHD) decreases the risk for substance abuse: findings from a longitudinal follow-up of youths with and without ADHD. J Clin Psychiatry. 2003. 64:Suppl 11. 3–8.11. Cox DJ, Merkel RL, Penberthy JK, Kovatchev B, Hankin CS. Impact of methylphenidate delivery profiles on driving performance of adolescents with attention-deficit/hyperactivity disorder: a pilot study. J Am Acad Child Adolesc Psychiatry. 2004. 43:269–275.
Article12. Greenhill LL, Pliszka S, Dulcan MK, Bernet W, Arnold V, Beitchman J, et al. Practice parameter for the use of stimulant medications in the treatment of children, adolescents, and adults. J Am Acad Child Adolesc Psychiatry. 2002. 41:26S–49S.
Article13. Connor DF. Preschool attention deficit hyperactivity disorder: a review of prevalence, diagnosis, neurobiology, and stimulant treatment. J Dev Behav Pediatr. 2002. 23:S1–S9.
Article14. Barkley RA. The use of psychopharmacology to study reciprocal influences in parent-child interaction. J Abnorm Child Psychol. 1981. 9:303–310.15. Barkley RA. The effects of methylphenidate on the interactions of preschool ADHD children with their mothers. J Am Acad Child Adolesc Psychiatry. 1988. 27:336–341.16. Barkley RA. Hyperactive girls and boys: stimulant drug effects on mother-child interactions. J Child Psychol Psychiatry. 1989. 30:379–390.17. Wilens TE, Biederman J. The stimulants. Psychiatr Clin North Am. 1992. 15:191–222.18. Newcorn JH, Kratochvil CJ, Allen AJ, Casat CD, Ruff DD, Moore RJ, et al. Atomoxetine and osmotically released methylphenidate for the treatment of attention deficit hyperactivity disorder: acute comparison and differential response. Am J Psychiatry. 2008. 165:721–730.
Article19. Clarke AR, Barry RJ, McCarthy R, Selikowitz M, Croft RJ. EEG differences between good and poor responders to methylphenidate in boys with the inattentive type of attention-deficit/ hyperactivity disorder. Clin Neurophysiol. 2002. 113:1191–1198.
Article20. Castellanos FX, Sonuga-Barke EJ, Milham MP, Tannock R. Characterizing cognition in ADHD: beyond executive dysfunction. Trends Cogn Sci. 2006. 10:117–123.
Article21. Castellanos FX, Sonuga-Barke EJ, Scheres A, Di Martino A, Hyde C, Walters JR. Varieties of attention-deficit/hyperactivity disorder-related intra-individual variability. Biol Psychiatry. 2005. 57:1416–1423.
Article22. de Zeeuw P, Aarnoudse-Moens C, Bijlhout J, König C, Post Uiterweer A, Papanikolau A, et al. Inhibitory performance, response speed, intraindividual variability, and response accuracy in ADHD. J Am Acad Child Adolesc Psychiatry. 2008. 47:808–816.
Article23. Doyle AE. Executive functions in attention-deficit/hyperactivity disorder. J Clin Psychiatry. 2006. 67:Suppl 8. 21–26.24. Klein C, Wendling K, Huettner P, Ruder H, Peper M. Intrasubject variability in attention-deficit hyperactivity disorder. Biol Psychiatry. 2006. 60:1088–1097.
Article25. Johnson KA, Kelly SP, Bellgrove MA, Barry E, Cox M, Gill M, et al. Response variability in attention deficit hyperactivity disorder: evidence for neuropsychological heterogeneity. Neuropsychologia. 2007. 45:630–638.
Article26. Hurks PP, Adam JJ, Hendriksen JG, Vles JS, Feron FJ, Kalff AC, et al. Controlled visuomotor preparation deficits in attention-deficit/hyperactivity disorder. Neuropsychology. 2005. 19:66–76.
Article27. Cheon KA, Ryu YH, Kim JW, Cho DY. The homozygosity for 10-repeat allele at dopamine transporter gene and dopamine transporter density in Korean children with attention deficit hyperactivity disorder: relating to treatment response to methylphenidate. Eur Neuropsychopharmacol. 2005. 15:95–101.
Article28. Bellgrove MA, Hawi Z, Kirley A, Gill M, Robertson IH. Dissecting the attention deficit hyperactivity disorder (ADHD) phenotype: sustained attention, response variability and spatial attentional asymmetries in relation to dopamine transporter (DAT1) genotype. Neuropsychologia. 2005. 43:1847–1857.
Article29. Kim YS, Cheon KA, Kim BN, Chang SA, Yoo HJ, Kim JW, et al. The reliability and validity of Kiddie-Schedule for Affective Disorders and Schizophrenia-Present and Lifetime Version-Korean version (K-SADS-PL-K). Yonsei Med J. 2004. 45:81–89.
Article30. Kwak K, Park H, Kim C. The manual for the Korean WISC-III. 2002. Seoul: The Special Education.31. So YK, Noh JS, Kim YS, Ko SG, Koh YJ. The reliability and validity of Korean parent and teacher ADHD rating scale. J Korean Neuropsychiatr Assoc. 2002. 41:283–289.32. Shin MS, Ryu ME, Kim BN, Hwang JW, Cho SC. Development of the Korean version of the IOWA Conners Rating Scale. J Korean Neuropsychiatr Assoc. 2005. 44:82–88.33. Arnold LE, Aman MG. Martin A, Scahill L, Charney DS, Leckman KF, editors. Clinical instruments and scales in pediatric psychopharmacology. Pediatric psychopharmacology. 2003. New York: Oxford University Press;412.34. Michelson D, Allen AJ, Busner J, Casat C, Dunn D, Kratochvil C, et al. Once-daily atomoxetine treatment for children and adolescents with attention deficit hyperactivity disorder: a randomized, placebo-controlled study. Am J Psychiatry. 2002. 159:1896–1901.
Article35. Shin M, Cho S, Chun S, Hong K. A study of the development and standardization of ADHD Diagnostic system. Korean J Child & Adol Psychiatr. 2000. 11:91–99.36. Bellgrove MA, Hester R, Garavan H. The functional neuroanatomical correlates of response variability: evidence from a response inhibition task. Neuropsychologia. 2004. 42:1910–1916.
Article37. Halperin JM, Trampush JW, Miller CJ, Marks DJ, Newcorn JH. Neuropsychological outcome in adolescents/young adults with childhood ADHD: profiles of persisters, remitters and controls. J Child Psychol Psychiatry. 2008. 49:958–966.
Article38. Naglieri JA, Goldstein S, Delauder BY, Schwebach A. Relationships between the WISC-III and the Cognitive Assessment System with Conners' rating scales and continuous performance tests. Arch Clin Neuropsychol. 2005. 20:385–401.
Article39. Losier BJ, McGrath PJ, Klein RM. Error patterns on the continuous performance test in non-medicated and medicated samples of children with and without ADHD: a meta-analytic review. J Child Psychol Psychiatry. 1996. 37:971–987.
Article40. Coghill DR, Rhodes SM, Matthews K. The neuropsychological effects of chronic methylphenidate on drug-naive boys with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2007. 62:954–962.
Article41. Johnson KA, Barry E, Bellgrove MA, Cox M, Kelly SP, Dáibhis A, et al. Dissociation in response to methylphenidate on response variability in a group of medication naïve children with ADHD. Neuropsychologia. 2008. 46:1532–1541.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- OROS Methylphenidate Treatment of Secondary Adult ADHD after Traumatic Brain Injury
- The Effectiveness of Methylphenidate in the Treatment of Encopresis Independent from Attention-Deficit Hyperactivity Disorder Symptoms
- Increased Cortisol after Stress is Associated with Variability in Response Time in ADHD Children
- A Review and an Update on Pharmacological Treatment of Children With Attention-Deficit/Hyperactivity Disorder
- Pharmacological treatment for attention deficit hyperactivity disorder in adults