Percutaneous Angioplasty of Portal Vein Stenosis that Complicates Liver Transplantation: The Mid-Term Therapeutic Results
- Affiliations
-
- 1Department of Radiology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Korea. swchoo@smc.samsung.co.kr
- KMID: 1102712
- DOI: http://doi.org/10.3348/kjr.2005.6.3.161
Abstract
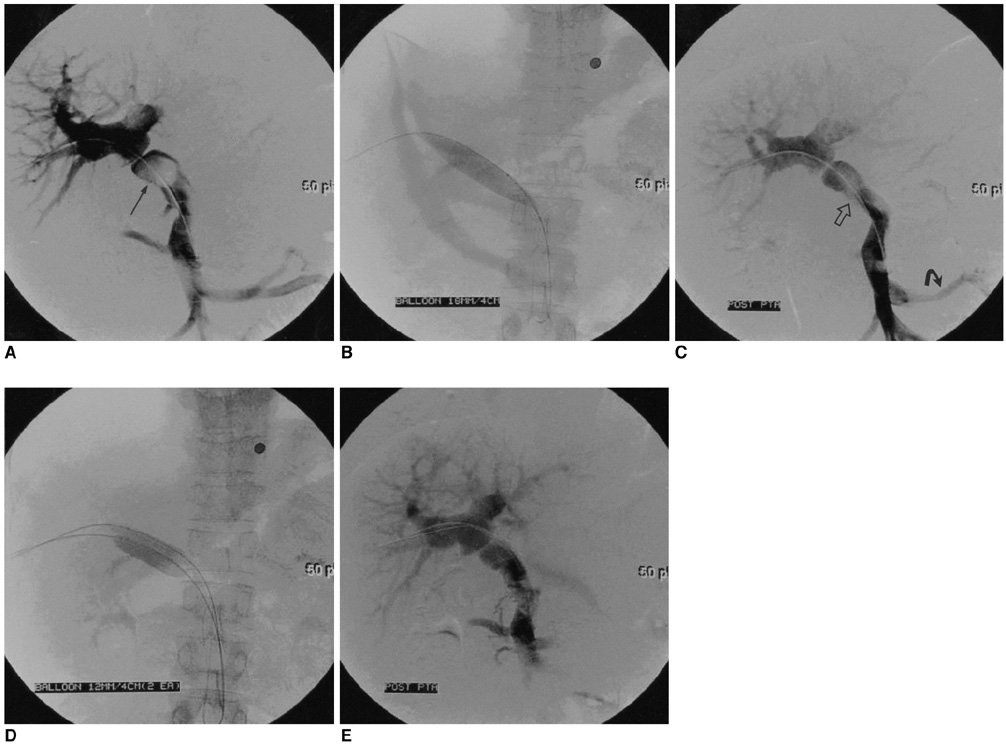
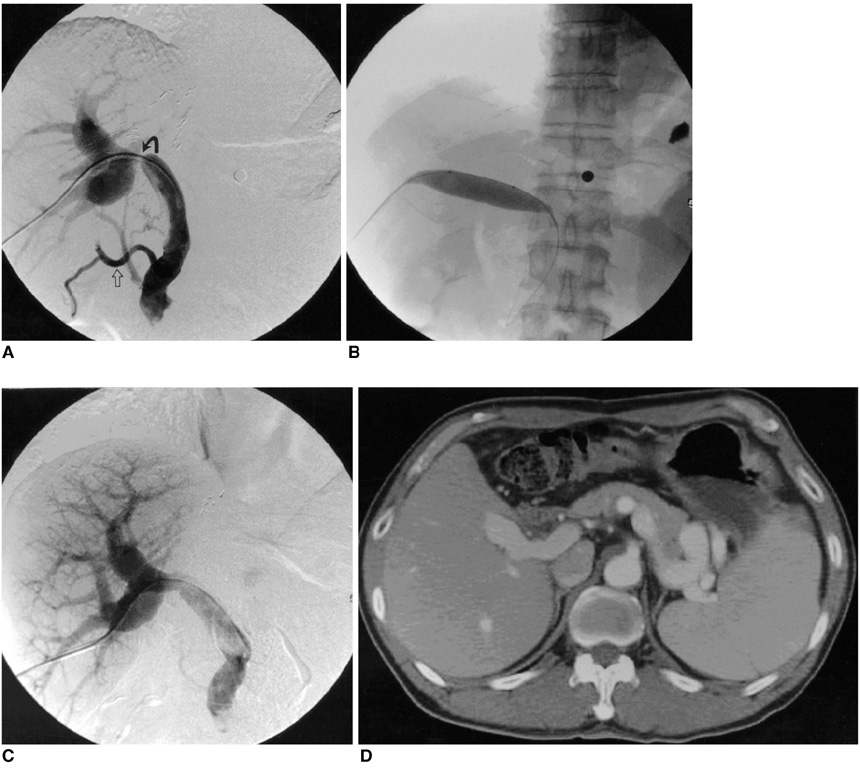
OBJECTIVE
We wanted to valuate the mid-term therapeutic results of percutaneous transhepatic balloon angioplasty for portal vein stenosis after liver transplantation. MATERIALS AND METHODS: From May 1996 to Feb 2005, 420 patients underwent liver transplantation. Percutaneous transhepatic angioplasty of the portal vein was attempted in six patients. The patients presented with the clinical signs and symptoms of portal venous hypertension or they were identified by surveillance doppler ultrasonography. The preangioplasty and postangioplasty pressure gradients were recorded. The therapeutic results were monitored by the follow up of the clinical symptoms, the laboratory values, CT and ultrasonography. RESULTS: The overall technical success rate was 100%. The clinical success rate was 83% (5/6). A total of eight sessions of balloon angioplasty were performed in six patients. The mean pressure gradient decreased from 14.5 mmHg to 2.8 mmHg before and after treatment, respectively. The follow up periods ranged from three months to 64 months (mean period; 32 months). Portal venous patency was maintained in all six patients until the final follow up. Combined hepatic venous stenosis was seen in one patient who was treated with stent placement. One patient showed puncture tract bleeding, and this patient was treated with coil embolization of the right portal puncture tract via the left transhepatic portal venous approach. CONCLUSION: Percutaneous transhepatic balloon angioplasty is an effective treatment for the portal vein stenosis that occurs after liver transplantation, and our results showed good mid-term patency with using this technique.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
Neoadjuvant chemotherapy followed by total pancreatectomy with splenectomy and combined vascular resections after preoperative percutaneous transhepatic portal vein stent placement in locally advanced pancreatic cancer with portal vein total obliteration
Yoonwon Kook, Munseok Choi, Jung Yup Park, Yong Eun Chung, Man-Deuk Kim, Woo Jung Lee, Chang Moo Kang
Ann Hepatobiliary Pancreat Surg. 2020;24(4):551-556. doi: 10.14701/ahbps.2020.24.4.551.Portal Vein Stenting for Delayed Jejunal Varix Bleeding Associated with Portal Venous Occlusion after Hepatobiliary and Pancreatic Surgery
Dongho Hyun, Kwang Bo Park, Sung Ki Cho, Hong Suk Park, Sung Wook Shin, Sung Wook Choo, Young Soo Do, In Wook Choo, Dong Wook Choi
Korean J Radiol. 2017;18(5):828-834. doi: 10.3348/kjr.2017.18.5.828.
Reference
-
1. Wozney P, Zajko AB, Bron KM, Point S, Starzl TE. Vascular complications after liver transplantation: a 5-year experience. AJR Am J Roentgenol. 1986. 147:657–663.2. Godoy MA, Camunez F, Echenagusia A, Simo G, Urbano J, Calleja J, et al. Percutaneous treatment of benign portal vein stenosis after liver transplantation. J Vasc Interv Radiol. 1996. 7:273–276.3. Buell JF, Funaki B, Cronin DC, Yoshida A, Perlman MK, Lorenz J, et al. Long-term venous complications after full-size and segmental pediatric liver transplantation. Ann Surg. 2002. 236:658–666.4. Vignali C, Cioni R, Petruzzi P, Cicorelli A, Bargellini I, Perri M, et al. Role of interventional radiology in the management of vascular complications after liver transplantation. Transplant Proc. 2004. 36:552–554.5. Funaki B, Rosenblum JD, Leef JA, Hackworth CA, Szymski GX, Alonso EM. Angioplasty treatment of portal vein stenosis in children with segmental liver transplants: mid-term results. AJR Am J Roentgenol. 1997. 169:551–554.6. Zajko AB, Sheng R, Bron K, Reyes J, Nour B, Tzakis A. Percutaneous transluminal angioplasty of venous anastomotic stenoses complicating liver transplantation: intermediate-term results. J Vasc Interv Radiol. 1994. 5:121–126.7. Lerut J, Tzakis AG, Bron K, Gordon RD, Iwatsuki S, Esquivel CO, et al. Complications of venous reconstruction in human orthotopic liver trnasplantation. Ann Surg. 1987. 205:404–414.8. Rollins NK, Sheffield EG, Andrews WS. Portal vein stenosis complicating liver transplantation in children: percutaneous transhepatic angioplasty. Radiology. 1992. 182:731–734.9. Scantlebury VP, Zajko AB, Esquivel CO, Marino IR, Starzl TE. Successful reconstruction of late portal stenosis after hepatic transplantation. Arch Surg. 1989. 124:503–505.10. Rouch DA, Emond JC, Ferrari M, Yousefzadeh D, Whitington P, Broelsch CE. The successful management of portal vein thrombosis after hepatic transplantation with splenorenal shunt. Surg Gynecol Obstet. 1988. 166:311–316.11. Funaki B, Rosenblum JD, Leef JA, Hackworth CA, Szymski GX, Alonso EM, et al. Portal vein stenosis in children with segmental liver transplants: treatment with percutaneous transhepatic venoplasty. AJR Am J Roentgenol. 1995. 165:161–165.12. Raby N, Karani J, Thomas S, O'Grady J, Williams R. Stenoses of vascular anastomoses after hepatic transplantation: treatment with balloon angioplasty. AJR Am J Roentgenol. 1991. 157:167–171.13. Funaki B, Rosenblum JD, Leef JA, Zaleski GX, Farrell T, Lorenz J, et al. Percutaneous treatment of portal venous stenosis in children and adolescents with segmental hepatic transplants: long-term results. Radiology. 2000. 215:147–151.14. Millis JM, Seaman DS, Piper JB, Alonso EM, Kelly S, Hackworth CA, et al. Portal vein thrombosis and stenosis in pediatric liver transplantation. Transplantation. 1996. 62:748.15. Denys A, Chevallier P, Doenz F, Qanadli SD, Sommacale D, Gillet M, et al. Interventional radiology in the management of complications after liver transplantation. Eur Radiol. 2004. 14:431–439.16. Bhattacharjya T, Olliff SP, Bhattacharjya S, Mirza DF, McMaster P. Percutaneous portal vein thrombolysis and endovascular stent for management of post transplant portal venous conduit thrombosis. Transplantation. 2000. 69:2195–2198.17. Baccarani U, Gasparini D, Risaliti A, Vianello V, Adani GL, Sainz M, et al. Percutaneous mechanical fragmentation and stent placement for the treatment of early post transplantation portal vein thrombosis. Transplantation. 2001. 72:1572–1582.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Living donor liver transplantation with pericholedochal collateral vein anastomosis in a pediatric patient with congenital absence of the portal vein
- Venous Complications after Pediatric Liver Transplantation
- Liver Transplantation in Liver Cirrhosis Patients Accompanied by Portal Vein Thrombosis
- Portal flow augmentation using meso-reno-portal anastomosis during liver transplantation with severe portal vein thrombosis
- Third retransplantation using a whole liver graft for late graft failure from hepatic vein stent stenosis in a pediatric patient who underwent split liver retransplantation