Korean J Radiol.
2010 Oct;11(5):560-565. 10.3348/kjr.2010.11.5.560.
Imaging Findings of Intrahepatic Bile Duct Adenoma (Peribiliary Gland Hamartoma): a Case Report and Literature Review
- Affiliations
-
- 1Department of Radiology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea. serha@catholic.ac.kr
- 2Department of Pathology, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- 3Department of Surgery, Seoul St. Mary's Hospital, College of Medicine, The Catholic University of Korea, Seoul 137-701, Korea.
- KMID: 1102582
- DOI: http://doi.org/10.3348/kjr.2010.11.5.560
Abstract
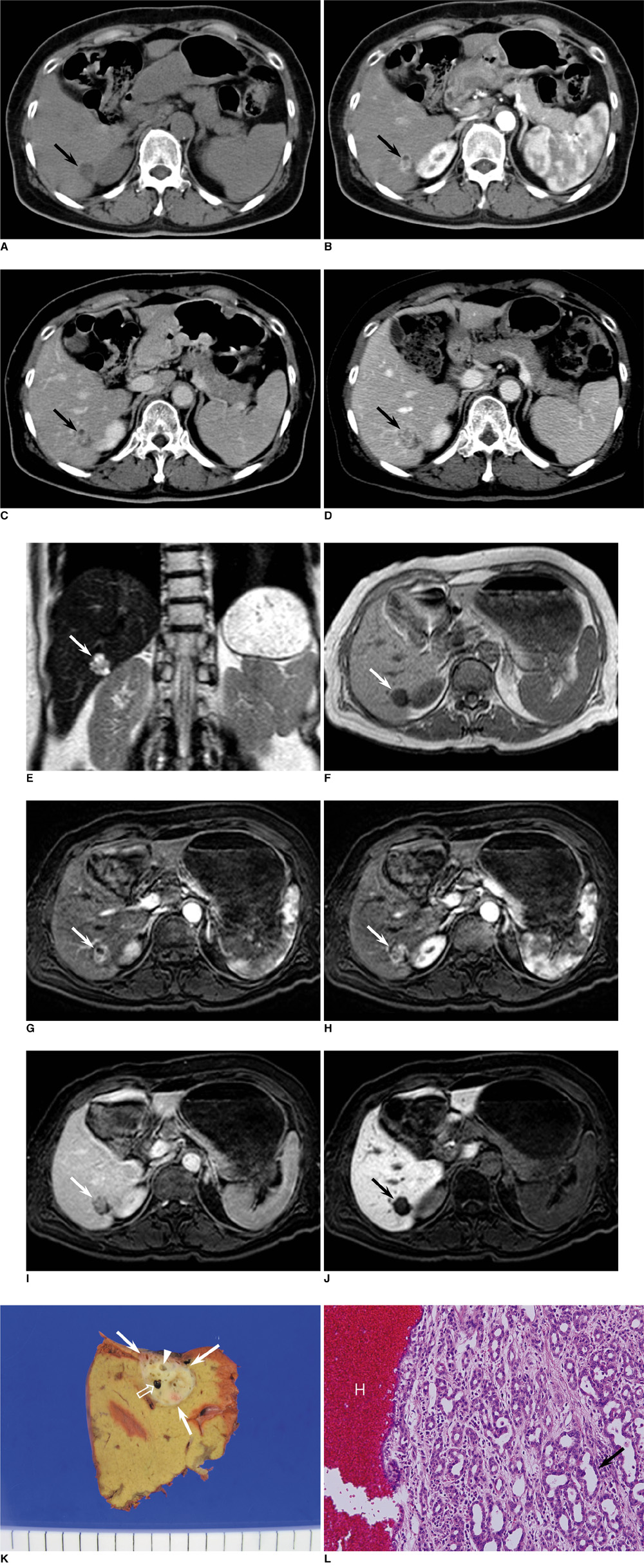
- Intrahepatic bile duct adenoma is a rare benign epithelial hepatic tumor derived from bile duct cells. We report the imaging findings of a patient with bile duct adenoma, which appeared as a small heterogeneously enhancing mass with focal small cystic change on CT and MRI. Follow-up images at seven months showed a slight increase in tumor size, which could be partly explained by intratumoral hemorrhage on pathologic examination. Although rare, bile duct adenoma should be considered as a differential diagnosis of a small hypervascular tumor located in the periphery of liver. Focal cystic change and intratumoral hemorrhage may occur.
MeSH Terms
Figure
Reference
-
1. Allaire GS, Rabin L, Ishak KG, Sesterhenn IA. Bile duct adenoma. A study of 152 cases. Am J Surg Pathol. 1998. 12:708–715.2. Edmondson HA. Tumors of the liver and intrahepatic bile duct. Atlas of tumor pathology. 1958. Washington DC: Armed Forces Institute of Pathology;19–29. fascicle 25.3. Craig JR, Peters RL, Edmondson HA. Tumors of the liver and intrahepatic bile ducts. Atlas of tumor pathology. 1989. Washington DC: Armed Forces Institute of Pathology;56–62. 2nd series, fascicle 26.4. Tajima T, Honda H, Kuroiwa T, Yoshimitsu K, Irie H, Aibe H, et al. Radiologic features of intrahepatic bile duct adenoma: a look at the surface of the liver. J Comput Assist Tomogr. 1999. 23:690–695.5. Cho C, Rullis I, Rogers LS. Bile duct adenoma as liver nodules. Arch Surg. 1978. 113:272–274.6. Hornick JL, Lauwers GY, Odze RD. Immunohistochemistry can help distinguish metastatic pancreatic adenocarcinomas from bile duct adenomas and hamartomas of the liver. Am J Surg Pathol. 2005. 29:381–389.7. Levin SE, Dail DH, Saik RP. Bile duct adenomatosis of the liver: a misleading finding on surgical exploration of the abdomen. Am Surg. 1975. 41:106–108.8. Christine AL, Elizabeth M. Gastrointestinal and Liver Pathology. 2005. Philadelphia, PA: Churchill Livingstone;600–602.9. Bhathal PS, Hughers NR, Goodman AD. The so-called bile duct adenoma is a peribiliary gland hamartoma. Am J Surg Pathol. 1996. 20:858–864.10. Semelka RC, Hussain SM, Marcos HB, Woosley JT. Biliary hamartomas: solitary and multiple lesions shown on current MR techniques including gadolinium enhancement. J Magn Reson Imaging. 1999. 10:196–201.11. Govindarajan S, Peters RL. The bile duct adenoma. A lesion distinct from Meyenburg complex. Arch Pathol Lab Med. 1984. 108:922–924.12. Kobayashi T, Matsui O, Takashima T. Abdominal Radiology Study Group of Japan. A case of bile duct adenoma (Japanese). Atlas of diagnostic abdominal imaging. 1993. vol. 1. Osaka, Japan: Nihon Schering;26–27.13. Miyazaki Y, Honda H, Yamamichi K. A case of bile duct adenoma, its features of preoperative imaging (Japanese). 1997. In : 33rd annual meeting of Liver Cancer Study Group; –175.14. Maeda E, Uozumi K, Kato N, Akahane M, Inoh S, Inoue Y, et al. Magnetic resonance findings of bile duct adenoma with calcification. Radiat Med. 2006. 24:459–462.15. Honda H, Onitsuka H, Yasumori K, Hayashi T, Ochiai K, Gibo M, et al. Intrahepatic peripheral cholangiocarcinoma: two-phased dynamic incremental CT and pathologic correlation. J Comput Assist Tomogr. 1993. 17:397–402.16. Seale MK, Catalano OA, Saini S, Hahn PF, Sahani DV. Hepatobiliary-specific MR contrast agents: role in imaging the liver and biliary tree. Radiographics. 2009. 29:1725–1748.17. Skelly RT, Lee J, Sloan JM, Diamond T. Incidental bile duct adenomas in a patient with obstructive jaundice. Ulster Med J. 1999. 68:114–115.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Peribiliary Cysts with Intrahepatic Bile Duct Obstruction: A Case Report
- Histopathology of a benign bile duct lesion in the liver: Morphologic mimicker or precursor of intrahepatic cholangiocarcinoma
- Diffusion-Weighted MRI in Intrahepatic Bile Duct Adenoma Arising from the Cirrhotic Liver
- Intrahepatic Bile Duct Dilatation Caused by Pancreatic Pseudocyst: A Case Report
- RE: Diffusion-Weighted MRI in Intrahepatic Bile Duct Adenoma Arising from the Cirrhotic Liver