Korean J Radiol.
2011 Dec;12(6):671-678. 10.3348/kjr.2011.12.6.671.
Lymphomatoid Granulomatosis: CT and FDG-PET Findings
- Affiliations
-
- 1Institute of Advanced Biomedical Imaging, National Jewish Health, Denver, CO 80206, USA. chungj@njhealth.org
- 2Department of Radiology, Massachusetts General Hospital, Boston, MA 02114, USA.
- 3Department of Pathology, Massachusetts General Hospital, Boston, MA 02114, USA.
- KMID: 1101920
- DOI: http://doi.org/10.3348/kjr.2011.12.6.671
Abstract
OBJECTIVE
Lymphomatoid granulomatosis (LG) is a rare, aggressive extranodal Epstein-Barr virus (EBV)-positive B-cell lymphoproliferative disease. The purpose of our study was to analyze the CT and fluorodeoxyglucose positron emission tomography (FDG-PET) findings of pulmonary LG.
MATERIALS AND METHODS
Between 2000 and 2009, four patients with pathologically proven pulmonary LG and chest CT were identified. Two of these patients also had FDG-PET. Imaging features of LG on CT and PET were reviewed.
RESULTS
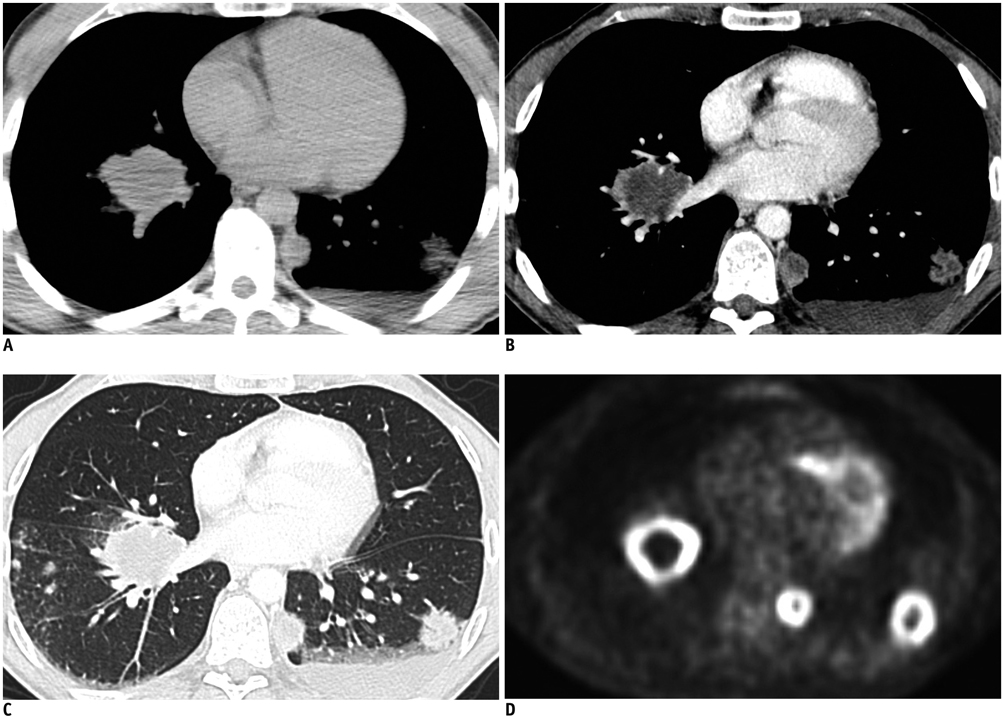
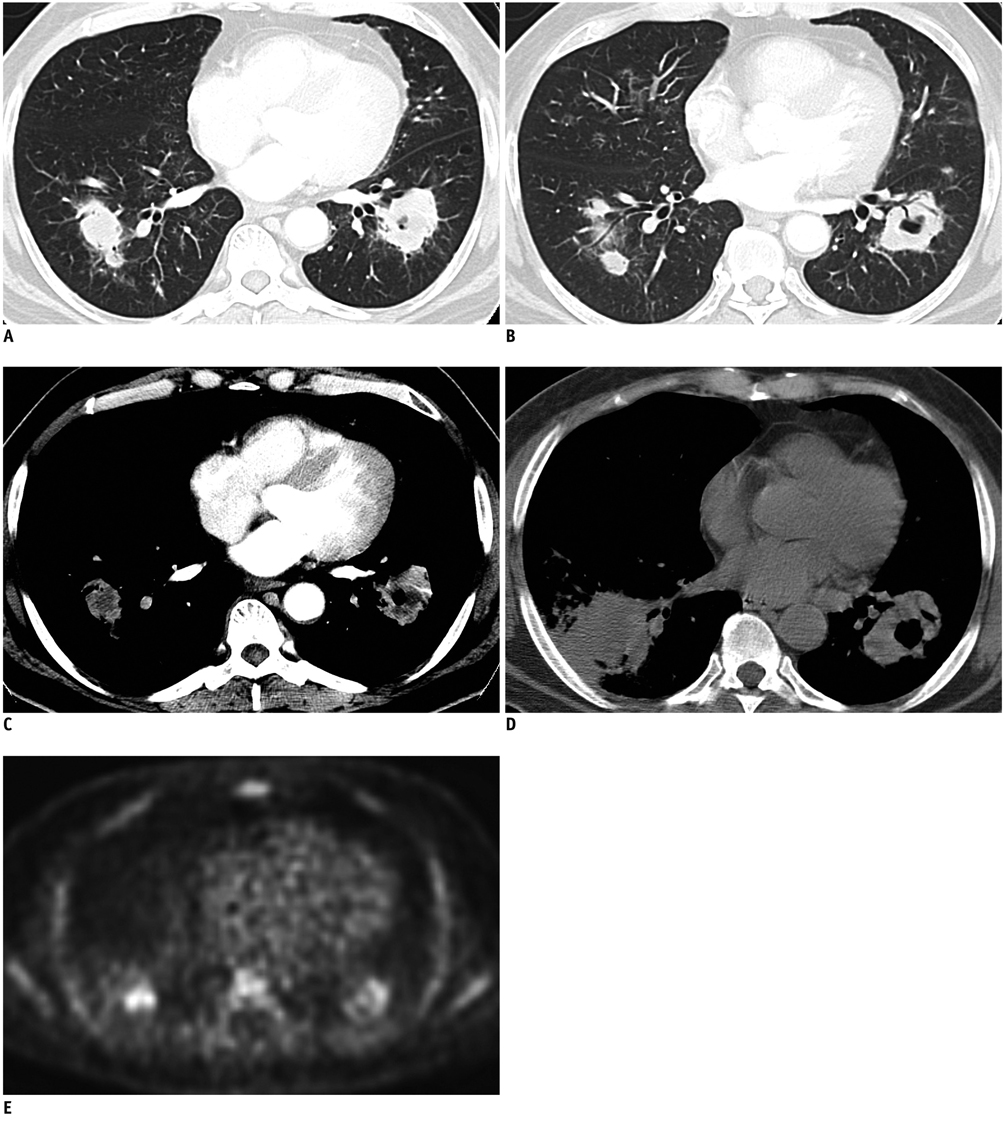
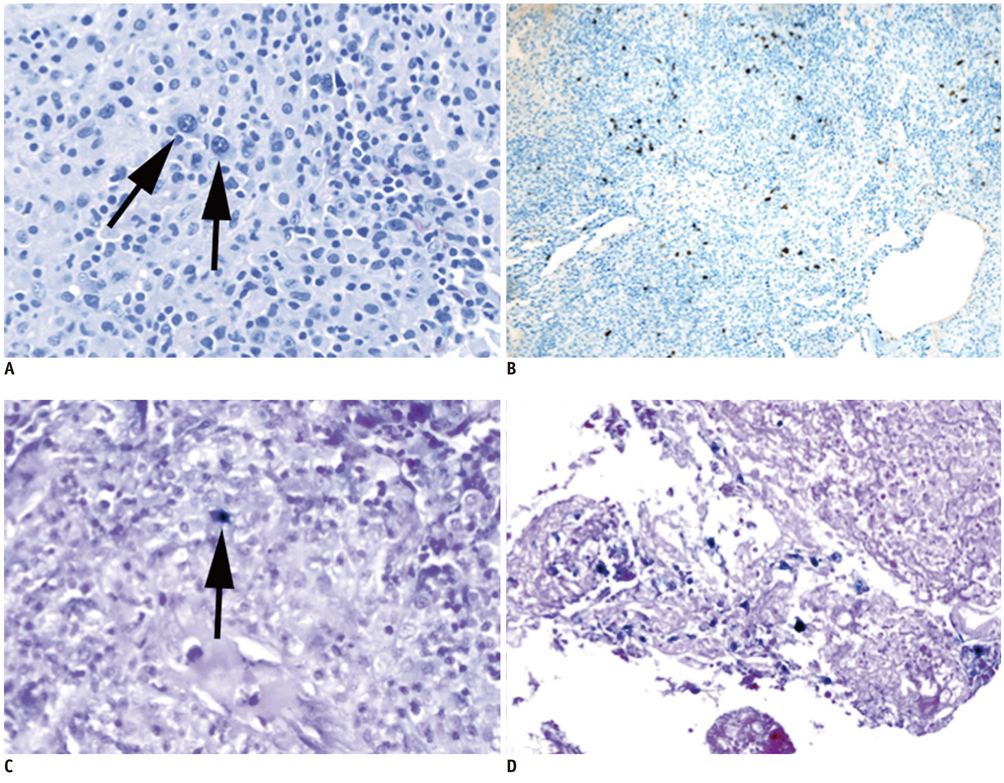
Pulmonary nodules or masses with peribronchovascular, subpleural, and lower lung zonal preponderance were present in all patients. Central low attenuation (4 of 4 patients), ground-glass halo (3 of 4 patients), and peripheral enhancement (4 of 4 patients) were observed in these nodules and masses. An air-bronchogram and cavitation were seen in three of four patients. FDG-PET scans demonstrated avid FDG uptake in the pulmonary nodules and masses.
CONCLUSION
Pulmonary LG presents with nodules and masses with a lymphatic distribution, as would be expected for a lymphoproliferative disease. However, central low attenuation, ground-glass halo and peripheral enhancement of the nodules/masses are likely related to the angioinvasive nature of this disease. Peripheral enhancement and ground-glass halo, in particular, are valuable characteristic not previously reported that can help radiologists suggest the diagnosis of pulmonary LG.
Keyword
MeSH Terms
-
Adult
Biopsy, Needle
Fluorodeoxyglucose F18/*diagnostic use
Humans
Lung Neoplasms/pathology/*radiography/*radionuclide imaging
Lymphomatoid Granulomatosis/pathology/*radiography/*radionuclide imaging
Male
Middle Aged
*Positron-Emission Tomography
Radiopharmaceuticals/*diagnostic use
*Tomography, X-Ray Computed
Figure
Reference
-
1. Guinee D Jr, Jaffe E, Kingma D, Fishback N, Wallberg K, Krishnan J, et al. Pulmonary lymphomatoid granulomatosis. Evidence for a proliferation of Epstein-Barr virus infected B-lymphocytes with a prominent T-cell component and vasculitis. Am J Surg Pathol. 1994. 18:753–764.2. Liebow AA, Carrington CR, Friedman PJ. Lymphomatoid granulomatosis. Hum Pathol. 1972. 3:457–558.3. Dee PM, Arora NS, Innes DJ Jr. The pulmonary manifestations of lymphomatoid granulomatosis. Radiology. 1982. 143:613–618.4. Hicken P, Dobie JC, Frew E. The radiology of lymphomatoid granulomatosis in the lung. Clin Radiol. 1979. 30:661–664.5. Wechsler RJ, Steiner RM, Israel HL, Patchefsky AS. Chest radiograph in lymphomatoid granulomatosis: comparison with Wegener granulomatosis. AJR Am J Roentgenol. 1984. 142:79–83.6. Prenovault JM, Weisbrod GL, Herman SJ. Lymphomatoid granulomatosis: a review of 12 cases. Can Assoc Radiol J. 1988. 39:263–266.7. Lee JS, Tuder R, Lynch DA. Lymphomatoid granulomatosis: radiologic features and pathologic correlations. AJR Am J Roentgenol. 2000. 175:1335–1339.8. Arai H, Oshiro H, Yamanaka S, Yukawa N, Wada N, Rino Y, et al. Grade I lymphomatoid granulomatosis with increased uptake of [18F] fluorodeoxyglucose in positron emission tomography: a case report. J Clin Exp Hematop. 2009. 49:39–44.9. Roarke MC, Nguyen BD. PET/CT characterization and monitoring of disease activity in lymphomatoid granulomatosis. Clin Nucl Med. 2007. 32:258–259.10. Rossi G, Marchioni A, Guicciardi N, Bertolini F, Valli R, Cavazza A. A rare cause of fever and PET-positive nodules in the lungs. Clin Respir J. 2009. 3:118–120.11. Pittaluga S, Jaffe ES. SH Swerdlow, Campo E, Harris NL, Jaffe ES, Pileri SA, Stein H, editors. Lymphomatoid granulomatosis. WHO classification of tumours of haematopoietic and lymphoid tissues. 2008. Lyon: IARC Press;247–249.12. Katzenstein AL, Carrington CB, Liebow AA. Lymphomatoid granulomatosis: a clinicopathologic study of 152 cases. Cancer. 1979. 43:360–373.13. Guinee DG Jr, Perkins SL, Travis WD, Holden JA, Tripp SR, Koss MN. Proliferation and cellular phenotype in lymphomatoid granulomatosis: implications of a higher proliferation index in B cells. Am J Surg Pathol. 1998. 22:1093–1100.14. Yamauchi Y, Yoshizawa A, Kudo K, Okuwaki H, Niino H, Morita T. [A case of lymphomatoid granulomatosis with multiple thin-walled cavities]. Nihon Kokyuki Gakkai Zasshi. 2002. 40:292–298.15. Vahid B, Salerno DA, Marik PE. Lymphomatoid granulomatosis: a rare cause of multiple pulmonary nodules. Respir Care. 2008. 53:1227–1229.16. Collins J. CT signs and patterns of lung disease. Radiol Clin North Am. 2001. 39:1115–1135.17. Kimura S, Ashizawa K, Matsuyama N, Kadota J, Kohno S, Hayashi K. [Imaging of Wegener's granulomatosis: changes by serial chest CT]. Nihon Kokyuki Gakkai Zasshi. 2002. 40:171–176.18. Wong JS, Weisbrod GL, Chamberlain D, Herman SJ. Bronchioloalveolar carcinoma and the air bronchogram sign: a new pathologic explanation. J Thorac Imaging. 1994. 9:141–144.19. Kui M, Templeton PA, White CS, Cai ZL, Bai YX, Cai YQ. Evaluation of the air bronchogram sign on CT in solitary pulmonary lesions. J Comput Assist Tomogr. 1996. 20:983–986.20. Lee YR, Choi YW, Lee KJ, Jeon SC, Park CK, Heo JN. CT halo sign: the spectrum of pulmonary diseases. Br J Radiol. 2005. 78:862–865.21. Benamore RE, Weisbrod GL, Hwang DM, Bailey DJ, Pierre AF, Lazar NM, et al. Reversed halo sign in lymphomatoid granulomatosis. Br J Radiol. 2007. 80:e162–e166.