Korean J Ophthalmol.
2007 Jun;21(2):100-105. 10.3341/kjo.2007.21.2.100.
The Results of B-scan Ultrasonography in Different Positions after Vitrectomy and Gas Tamponade
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University College of Medicine, Seoul, Korea. wismile@unitel.co.kr
- KMID: 1101912
- DOI: http://doi.org/10.3341/kjo.2007.21.2.100
Abstract
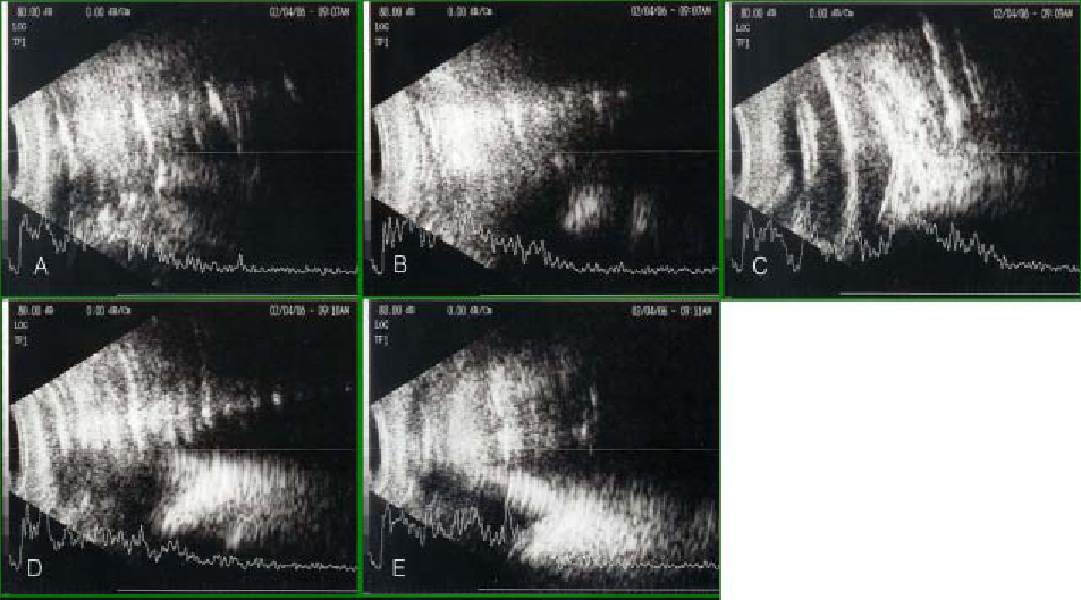
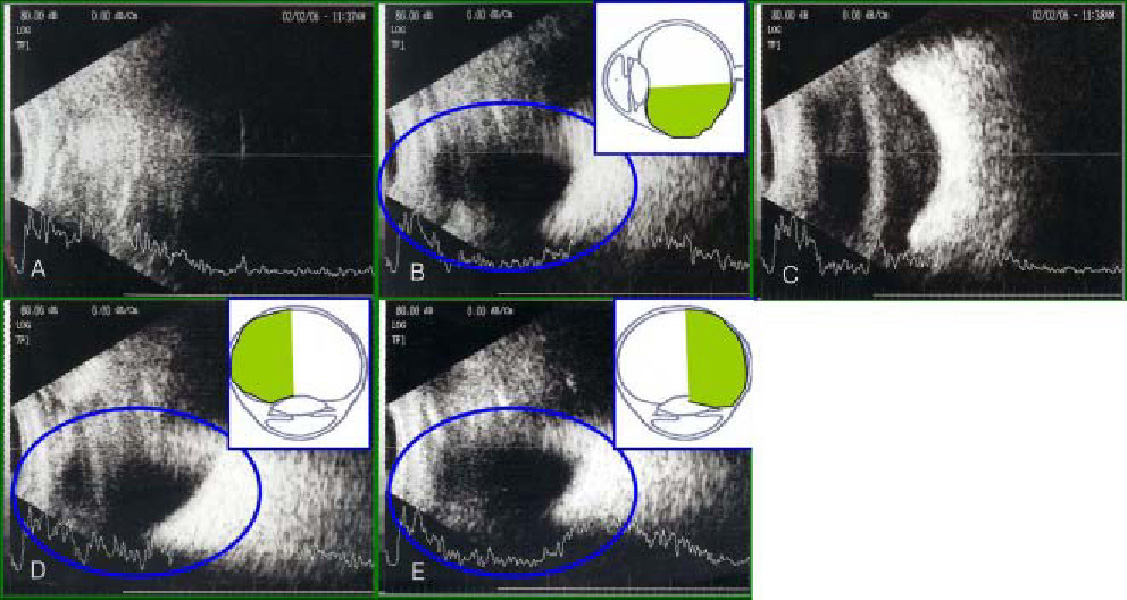
- PURPOSE: To determine the proper time frame in which to assess retinal attachment status and to evaluate the superior retinal attachment status by performing B-scan ultrasonography in different positions on patients who have undergone pars plana vitrectomy and gas tamoponade. METHODS: In this prospective study, 23 patients (23 eyes) who had undergone pars plana vitrectomy and gas tamponade were investigated between June 2005 and February 2006. SF6 (18%) was injected into the vitreous cavity of 15 eyes, and C3F8 (14%) was injected into the vitreous cavity of 8 eyes. At postoperative day 1, day 3, week 1, week 2, and week 4, B-scan ultrasonography was performed in the supine, sitting, prone, right decubitus, and left decubitus positions. RESULTS: The proper time to evaluate the retinal attachment status was three days post-operatively in 10 eyes (66.7%) with SF6 (18%) injections and two weeks post-operatively in six eyes (75%) that had C3F8 (14%) injections. The superior retinal attachment status can be evaluated from the summation of B-scan ultrasonography results performed in the right decubitus and left ducubitus positions. CONCLUSIONS: The proper time to evaluate the retinal attachment status was related to the degree of the gas absorption when performing B-scan ultrasonography after pars plana vitrectomy and gas tamponade. To evaluate the entire retina, it is useful to perform B-scan ultrasonograhy in the prone, right decubitus and left decubitus positions.
Keyword
MeSH Terms
Figure
Reference
-
1. Susanne S, Katharina K, Andreas W. Incidence of rhegmatogenous retinal detachment after vitrectomy in eyes of diabetic patients. Retina. 2006. 26:149–152.2. Han NS, Lee SB, Jo YJ. The results of primary vitrectomy for rhegmatogenous retinal detachment. J Korean Ophthalmol Soc. 2006. 47:55–61.3. Ahn JB, Huh K. Clinical analysis of vitrectomy for complication of proliferative diabetic retinopathy. J Korean Ophthalmol Soc. 1996. 37:1161–1167.4. Mochizuki Y, Yubota T, Hata Y, et al. Surgical results of combined pars plana vitrectomy, phacoemulsification, and intraocular lens implantation. Eur J Ophthalmol. 2006. 16:279–286.5. Treumer F, Bunse A, Rudolf M, Roider J. Pars plana vitrectomy, phacoemulsification and intraocular lens implantation. Comparison of clinical complications in a combined versus two-step surgical approach. Graefes Arch Clin Exp Ophthalmol. 2006. 244:808–815.6. Stephen JR, Ronald L, Green , Sandra FB. Diagnostic ophthalmic ultrasound. Retina. 2006. v. 1:4th ed. Baltimore: Elsevier Mosby;chap. 19.7. Wong Raymond F, Thomson John T. Prediction of the kinetics of disapperance of sulfur hexafluoride and perfluoropropane intraocular gas bubbles. Ophthalmology. 1988. 95:609–613.8. Thomson JT. Kinetics of intraocular gases. Arch Ophthalmol. 1989. 107:687–691.9. Lincoff H, Maise JM, Lincoff A. Intravitreal disappearance rates of four perfluorocarbon gases. Arch Ophthalmol. 1984. 102:928–929.10. Whitacre Macr M. B-scan ultrasonograghy of eyes containing intravitreal gas. Am J Ophthalmol. 1991. 112:272–277.11. Laing FC. Commonly encountered artifacts in clinical ultrasound. Seminars In Ultrasound. 1983. 4:27.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Postural Effect on Intraocular Pressure in Gas-Filled Eyes after Vitrectomy
- Postoperative Refractive Error after Vitrectomy In Macular Hole Patients
- The Change in Corneal Endothelial Cell Density after Pars Plana Vitrectomy
- Postoperative Refractive Error by Using A-scan in Cataract Surgery After Vitrectomy
- The Effect of Gas Tamponade with Vitrectomy in Lamellar Macular Hole