Korean J Radiol.
2008 Jul;9(Suppl):S65-S67. 10.3348/kjr.2008.9.s.s65.
The Rare Association of Moyamoya Disease and Cerebral Arteriovenous Malformations: a Case Report
- Affiliations
-
- 1Department of Radiology, Chi-Mei Foundation Hospital, Taipei, Taiwan. wyguo@vghtpe.gov.tw
- 2Department of Radiology, Taipei Veterans General Hospital, Taipei, Taiwan.
- 3National Yang-Ming University School of Medicine, Taipei, Taiwan.
- 4Cancer Center, Taipei Veterans General Hospital, Taipei, Taiwan.
- 5Neurological Institute, Taipei Veterans General Hospital, Taipei, Taiwan.
- KMID: 1100108
- DOI: http://doi.org/10.3348/kjr.2008.9.s.s65
Abstract
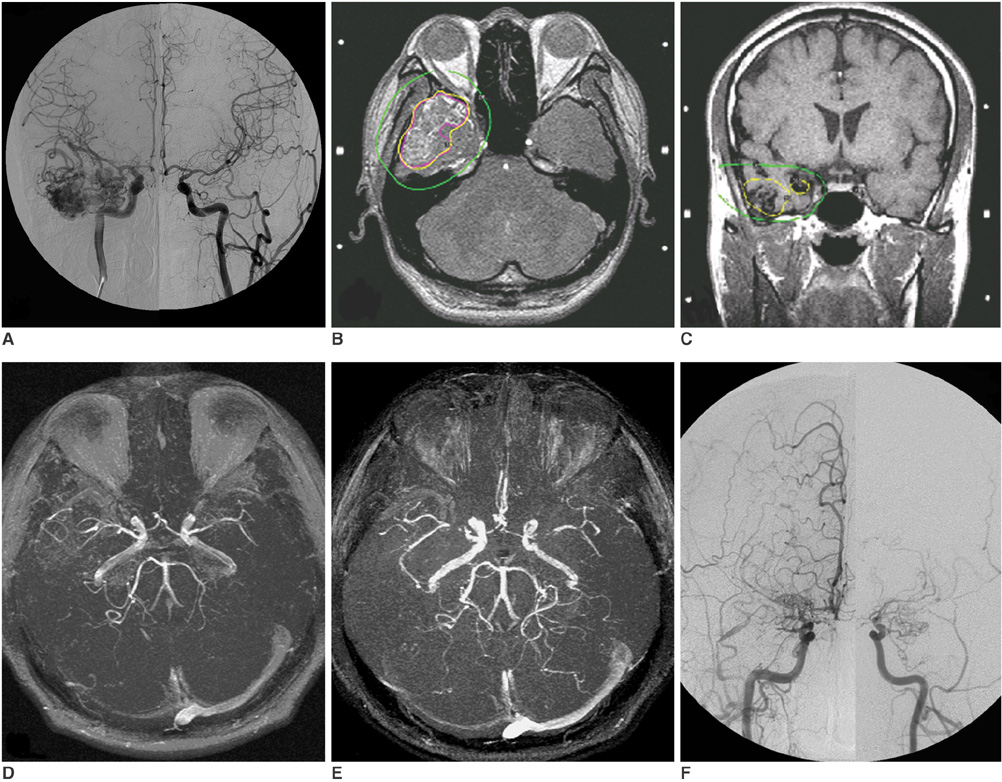
- A 36-year-old man was diagnosed with a right temporal lobe grade II cerebral arteriovenous malformation (cAVM) and was treated with radiosurgery. At nine months after the cAVM radiosurgery, the patient began to develop bilateral focal narrowing at the M1 segments of the bilateral middle cerebral arteries. The narrowing progressively deteriorated as was demonstrated on longitudinal serial follow-up MR imaging. X-ray angiography performed at 51 months after radiosurgery confirmed that the cAVM was cured and a diagnosis of moyamoya disease. To the best of our knowledge, this is the first case of cAVM-associated moyamoya disease that developed after radiosurgery. Given the chronological sequence of disease development and radiation dose distribution of radiosurgery, it is proposed that humoral or unknown predisposing factors, rather than direct radiation effects, are the cause of moyamoya disease associated with cAVM.
MeSH Terms
Figure
Reference
-
1. Mawad ME, Hilal SK, Michelsen WJ, Stein B, Ganti SR. Occlusive vascular disease associated with cerebral arteriovenous malformations. Radiology. 1984. 153:401–408.2. Enam SA, Malik GM. Association of cerebral arteriovenous malformations and spontaneous occlusion of major feeding arteries: clinical and therapeutic implications. Neurosurgery. 1999. 45:1105–1111.3. Söderman M, Guo WY, Karlsson B, Pelz DM, Ulfarsson E, Andersson T. Neurovascular radiosurgery. Interventional Neuroradiology. 2006. 12:189–202.4. Nakashima T, Nakayama N, Furuichi M, Kokuzawa J, Murukawa T, Sakai N. Arteriovenous malformation in association with moyamoya disease Report of two cases. Neurosurg Focus. 1998. 5:E6.5. Halatsch ME, Rustenbeck HH, Jansen J. Progression of arteriovenous malformation in moyamoya syndrome. Acta Neurochir (Wien). 1997. 139:82–85.6. Seol HJ, Kim DG, Oh CW, Han DH. Radiosurgical treatment of a cerebral arteriovenous malformation in a patient with moyamoya disease: case report. Neurosurgery. 2002. 51:478–482.7. Montanera W, Marotta TR, terBrugge KG, Lasjaunias P, Willinsky R, Wallace MC. Cerebral arteriovenous malformations associated with moyamoya phenomenon. AJNR Am J Neuroradiol. 1990. 11:1153–1156.8. Schmit BP, Burrows PE, Kuban K, Goumnerova L, Scott RM. Acquired cerebral arteriovenous malformation in a child with moyamoya disease: case report. J Neurosurg. 1996. 84:677–680.9. Fuse T, Takagi T, Fukushima T, Hashimoto N, Yamada K. Arteriovenous malformation associated with moyamoya disease. Childs Nerv Syst. 1996. 12:404–408.10. Pincus DW, Choudhri T, Feldstein NA, Sisti MB, Stein BM. Moyamoya syndrome following stereotactic radiosurgery for AVM (abstract of oral presentation in the 1997 Annual Meeting of the Congress of Neurological Surgeons). Neurosurgery. 1997. 4:731.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Probable Moyamoya Disease (Unilateal Moyamoya Disease) Coexisting Arteriovenous Malformation
- Arteriovenous Malformation with an Occlusive Feeding Artery Coexisting with Unilateral Moyamoya Disease
- Intracranial Lesions Associated with Cerebral Aneurysms
- A Case of Moyamoya Disease Associated with Complete Duplication of the Basilar artery
- Cerebral Arteriovenous Malformation Associated with Moyamoya Disease