Korean J Ophthalmol.
2005 Mar;19(1):80-83. 10.3341/kjo.2005.19.1.80.
Acquired Simulated Brown Syndrome following Surgical Repair of Medial Orbital Wall Fracture
- Affiliations
-
- 1Department of Ophthalmology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. htlim@amc.seoul.kr
- KMID: 1099091
- DOI: http://doi.org/10.3341/kjo.2005.19.1.80
Abstract
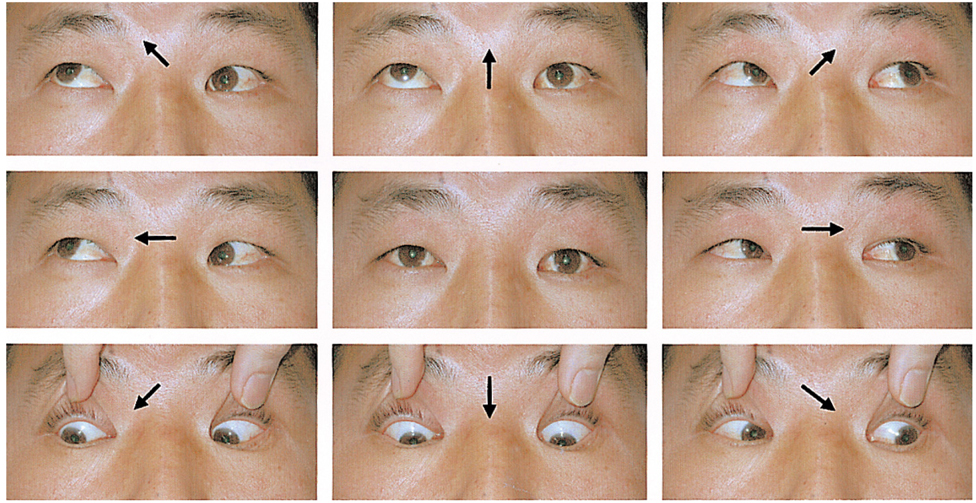
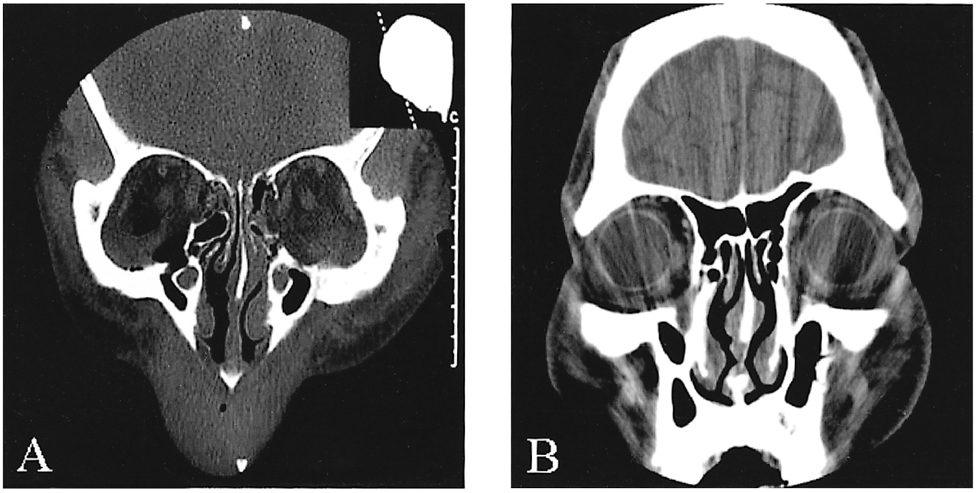
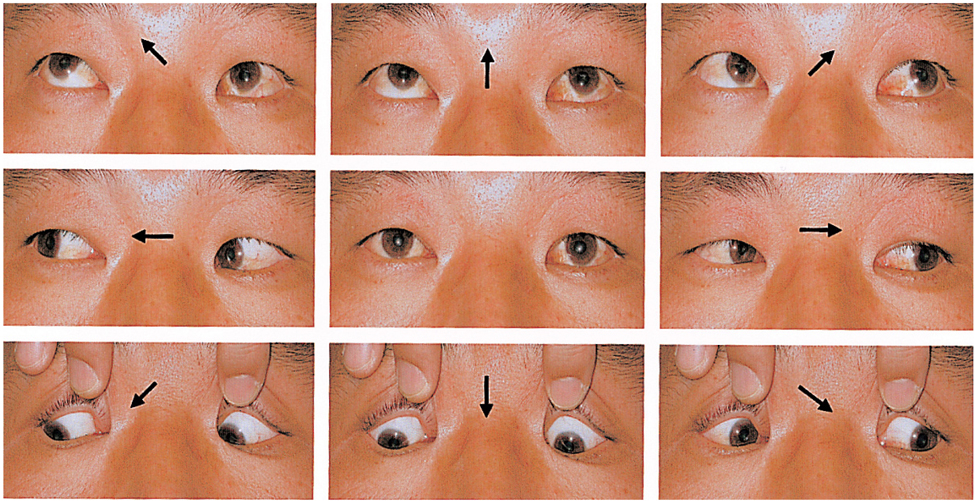
- Simulated Brown syndrome is a term applied to a myriad of disorders that cause a Brown syndrome-like motility. We encountered a case of acquired simulated Brown syndrome in a 41-year-old man following surgical repair of fractures of both medial orbital walls. He suffered from diplopia in primary gaze, associated with hypotropia of the affected eye. We performed an ipsilateral recession of the left inferior rectus muscle as a single-stage intraoperative adjustment procedure under topical anesthesia, rather than the direct approach to the superior oblique tendon. Postoperatively, the patient was asymptomatic in all diagnostic gaze positions.
Keyword
MeSH Terms
-
Adult
Anesthesia, Local
Diplopia/*etiology/surgery
Eye Movements
Humans
Male
Ocular Motility Disorders/*etiology/radiography/surgery
Oculomotor Muscles/surgery
Ophthalmologic Surgical Procedures
Orbital Fractures/radiography/*surgery
*Postoperative Complications
Strabismus/etiology/surgery
Tomography, X-Ray Computed
Vision, Binocular
Figure
Reference
-
1. Brown HW. Allen JH, editor. Congenital structural anomalies of the muscle. Symposium on strabismus, Trans New Orleans Acad Ophthalmol. 1950. St Louis: CV Mosby;205–236.2. Wilson ME, Eutis HS Jr, Parks MM. Brown's syndrome. Surv Ophthalmol. 1989. 34:153–172.3. Erie JC. Acquired Brown's syndrome after peribulbar anesthesia. Am J Ophthalmol. 1990. 109:349–350.4. Zipf RF, Trokel SL. Simulated superior oblique tendon sheath syndrome following orbital floor fracture. Am J Ophthalmol. 1973. 75:700–705.5. Lauer SA, Sauer H, Pak SM. Brown's syndrome diagnosed following repair of an orbital roof fracture: a case report. J Craniomaxillofac Trauma. 1998. 4:20–22.6. Baker RS, Conklin JD. Acquired Brown's syndrome from blunt orbital trauma. J Pediatr Ophthalmol Strabismus. 1987. 24:17–21.7. Crawford JS. Surgical treatment of true Brown's syndrome. Am J Ophthalmol. 1976. 81:289–295.8. Wright KW. Superior oblique silicone expander for Brown syndrome and superior oblique overaction. J Pediatr Ophthalmol Strabismus. 1991. 28:101–107.9. Stager DR Jr, Parks MM, Stager DR Sr. Long-term results of silicone expander for moderate and severe Brown syndrome (Brown syndrome "plus"). J AAPOS. 1999. 3:328–332.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Acquired Brown Syndrome after Surgical Repair of a Medial Orbital Wall Fracture
- Repair of Orbital Wall Fracture Using Transcaruncular Approach
- Three Cases of Acquired Simulated Brown Syndrome after Blowout Fracture Operations
- Transcaruncular Approach to Blowout Fractures of the Medial Orbital Wall
- The Direct Medial Canthal Approach in the Repair of Blowout Fracture of the Medial Orbital Wall