Korean J Ophthalmol.
2010 Feb;24(1):4-9. 10.3341/kjo.2010.24.1.4.
Lower Eyelid Epiblepharon Associated with Lower Eyelid Retraction
- Affiliations
-
- 1Department of Ophthalmology, Inje University Sanggye Paik Hospital, Seoul, Korea.
- 2Department of Ophthalmology, Seoul National University Hospital, Seoul, Korea. khwarg@snu.ac.kr
- 3Department of Ophthalmology, Seoul National University Boramae Hospital, Seoul, Korea.
- 4Department of Ophthalmology, Seoul National University Bundang Hospital, Seongnam, Korea.
- KMID: 1098786
- DOI: http://doi.org/10.3341/kjo.2010.24.1.4
Abstract
-
PURPOSE: To describe a series of patients with lower eyelid epiblepharon associated with lower eyelid retraction.
METHODS
We retrospectively reviewed the medical records of patients who underwent surgery for lower eyelid retraction, epiblepharon, or thyroid-associated ophthalmopathy (TAO) between October 1999 and March 2007. Patients with both lower eyelid retraction and epiblepharon on preoperative examination were included in this study.
RESULTS
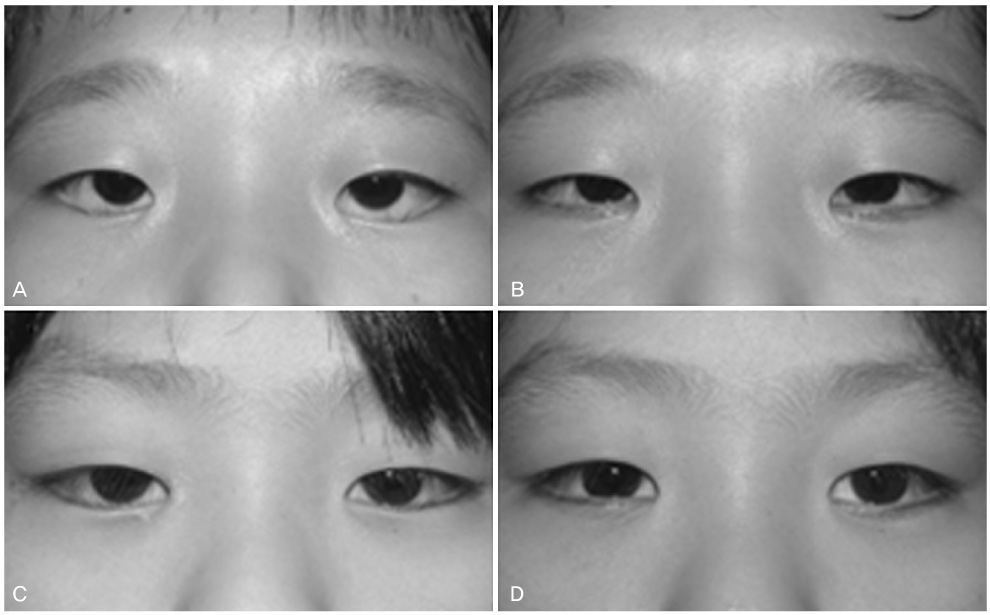
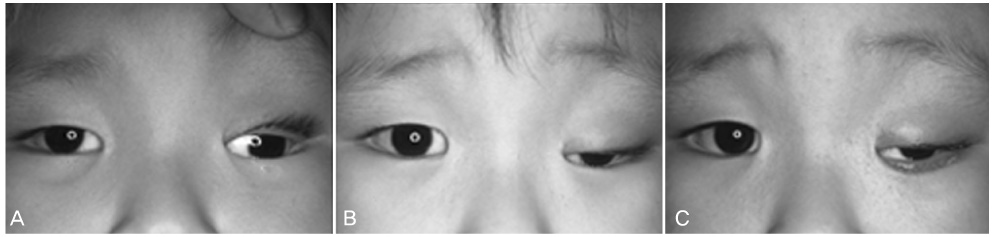
Twenty-seven eyelids of 20 patients with both lower eyelid retraction and epiblepharon were enrolled. The underlying causes of lower eyelid retraction included congenital retraction (seven eyelids), congenital fibrosis of the extraocular muscles (CFEOM; seven eyelids), TAO (seven eyelids), post-operative cicatricial retraction (five eyelids), and facial nerve palsy (one eyelid). Eight of 27 eyelids were successfully corrected after the repair of retraction without the repair of epiblepharon, regardless of the cause of lower eyelid retraction. Another four eyelids with epiblepharon associated with TAO resolved after only orbital decompression. Cilia-everting sutures were additionally applied for epiblepharon in another 14 eyelids, 12 of which did not require the excision of a skin fold or the orbicularis muscles. Only one eyelid with mild retraction and epiblepharon underwent simple epiblepharon repair. Recurrence of retraction or epiblepharon developed in three eyelids during follow-up.
CONCLUSIONS
In cases with both lower eyelid retraction and epiblepharon, the retraction should be repaired first, and then the epiblepharon can be corrected selectively according to the severity of the case.
Keyword
MeSH Terms
Figure
Reference
-
1. Chang EL, Rubin PA. Upper and lower eyelid retraction. Int Ophthalmol Clin. 2002. 42(2):45–59.2. Bosniak S. Principles and practice of ophthalmic plastic and reconstructive surgery. 1996. Philadelphia: WB Saunders;438–466.3. Chang EL, Hayes J, Hatton M, Rubin PA. Acquired lower eyelid epiblepharon in patients with thyroid eye disease. Ophthal Plast Reconstr Surg. 2005. 21:192–196.4. Moon JW, Choung HK, Khwarg SI. Correction of lower lid retraction combined with entropion using an ear cartilage graft in the anophthalmic socket. Korean J Ophthalmol. 2005. 19:161–167.5. Collin JR, Allen L, Castronuovo S. Congenital eyelid retraction. Br J Ophthalmol. 1990. 74:542–544.6. Harley RD, Rodrigues MM, Crawford JS. Congenital fibrosis of the extraocular muscles. J Pediatr Ophthalmol Strabismus. 1978. 15:346–358.7. Woo KI, Yi K, Kim YD. Surgical correction for lower lid epiblepharon in Asians. Br J Ophthalmol. 2000. 84:1407–1410.8. Khwarg SI, Choung HK. Epiblepharon of the lower eyelid: technique of surgical repair and quantification of excision according to the skin fold height. Ophthalmic Surg Lasers. 2002. 33:280–287.9. Park RI, Meyer DR. Acquired lower eyelid epiblepharon. Am J Ophthalmol. 1996. 122:449–451.10. Roh YB, Kim JH, Oum BS, Baek SY. Clinical and histological study of extraocular muscle in congenital fibrosis syndrome. J Korean Ophthalmol Soc. 1996. 37:1907–1914.11. Cockerham KP, Hidayat AA, Brown HG, et al. Clinicopathologic evaluation of the Mueller muscle in thyroid-associated orbitopathy. Ophthal Plast Reconstr Surg. 2002. 18:11–17.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Outcomes of Various Surgical Procedures on Acquired Lower Eyelid Epiblepharon in Thyroid Associated Ophthalmopathy
- Clinical Outcomes of Lower Eyelid Epiblepharon Repair Combined with Minimal Incision of Medial Epicanthoplasty
- Epiblepharon of the lower eyelid: classification and association with astigmatism
- Surgical Efficacyin the Upper and Lower Eyelid Retraction
- Acellular Dermal Allograft for the Correction of Eyelid Retraction